
Vitamin B12 Deficiency in Autism
-
Vitamin B12 loading of the brain happens predominantly in the womb, with little more vitamin B12 loading of the brain for the rest of life
-
Vitamin B12 loading of the brain increases progressively as the foetus matures.
-
Premature babies have lower brain vitamin B12.
-
Vitamin B12 deficiency during pregnancy leads to vitamin B12 deficiency in the neonate
-
Vitamin B12 deficiency in the neonate is associated with delayed physical and mental development.
-
Vitamin B12 deficiency during pregnancy increases the risk for preterm labour, low birth weight and increased infant mortality.
-
The brains of children with autism have been found to have greatly reduced levels of vitamin B12.
-
All children with ASD have been found to be functionally deficient in vitamin B12 at time of assessment
-
Vitamin B12 deficiency in the neonate can be associated with hypotonia
-
Vitamin B12 deficiency is associated with reduced aconitase activity, which is associated with a lower Mini Mental Score
-
Vitamin B12 deficiency in the mothers during pregnancy is known to cause severe retardation of myelination of the nervous system of the foetus.
-
Vitamin B12 deficiency during development is associated with delay in the development of speech
-
Inadequate myelination in the various regions of the brain is common in children with autism
-
Vitamin B12 deficiency reduces the production of melatonin in the child and is associated with sleep disorders in ASD
-
Vitamin B12 deficiency reduces the production of gut melatonin and is associated with poor intestinal health, lactose intolerance and multiple food intolerance.
-
Vitamin B12 deficiency has been associated with epilepsy in children with ASD
-
Paradoxical B12 deficiency is common in children with ASD
-
Children with Pardoxical B12 deficiency do not respond to cyanocobalamin and require resolution of functional B2 deficiency before functional B12 deficiency can be resolved
Nutritional Sufficiency of Children
The maternal decision to carry a child to term creates a beneficence-based fiduciary obligation on the part of the mother (and physician) to act in the best interest of the unborn child, and to sacrificially care for and nurture that child, There can be no doubt that this extends to ensuring nutritional sufficiency of the child in its early life. (Centre for Bioethics) Unfortunately the vitamin B12 status of women in pregnancy is often not measured, and conditions such as Paradoxical B12 insufficiency are very poorly understood. Nor are the potential consequences of vitamin B12 deficiency in the mother and neonate explained to the pregnant mother.
Vitamin B12 Deficiency in Neonates
Nutritional B12 deficiency is a treatable cause of neurodevelopmental delay in infants (Acıpayam etal, 2020).
Infants born with cobalamin (vitamin B12) deficiency are at significant risk of lasting brain damage. Further, the deficiency can cause development and intellectual delay, hypotonia, tremor, seizure, and failure to thrive. In addition the children may have speech, linguistics and social impairments, as well as behavioural disorders, and problems with fine and gross motor movement. Without therapy, there can be irreversible intellectual impairment, as well as cognitive and developmental delay (Hasbaoui etal, 2021). Of these the concurrence of hypotonia with developmental and intellectual delay, especially with premature birth, low birth weight, difficulties feeding, and problems sleeping are all "Red Flags" for Vitamin B12 deficiency. They are also all associated with autism. It is almost unbelievable that despite countless publications on the effects of vitamin B12 deficiency in the neonate that this association with autism is missed. In overt B12 deficiency, "Neurological findings and developmental delay related to nutritional B12 deficiency can be prevented without sequelae if diagnosed early" (Acıpayam etal, 2020). Despite this functional vitamin B12 deficiency in children is frequently mis-diagnosed.It is almost unbelievable that despite countless publications on the effects of vitamin B12 deficiency in the neonate that this association with autism is missed by the medical profession, who do not test for metabolic makers of vitamin B12 deficiency, such as homocysteine, and MMA..Vitamin B12 Deficiency and Hypotonia
Identification of hypotonia in neonates is a strong indication of potential vitamin B12 deficiency (either absolute or paradoxical) (Chalouhi et al, 2008; Demir et al, 2013; Bousselamti et al, 2018;Payam et al, 2020; Akcaboy etal, 2015; Serin et al, 2019; Incecik et al, 2010; Honzik et al, 2010; Bicakci 2015; Smolka etal, 2001; Taskesen et al, 2011; Gupta et al, 2019; Benbir etal, 2007; Vieira etal, 2020; Ma etal, 2011; Borkowska etal 2007; Wagnon etal, 2005; Kamoun etal, 2017; Tosun etal, 2011; Kose etal, 2020; Lövblad etal, 1997; Lücke etal, 2007; Hall 1990; Vieira etal, 2020; Taskesen etal, 2011; Serin etal, 2015; Bicakci 2015; Serin HM, Arslan , 2019; Aguirre etal, 2019; Casella etal, 2005; Acıpayam etal, 020; Bousselamti etal, 2018;Hasbaoui etal, 2021 Hypotonia, is very common in autism, and early diagnosis of autism should be suspected in children with hypotonia, as "Hypotonia is a recognizable marker of ASD and should serve as a "red flag" to prompt earlier recognition and neurodevelopmental evaluation toward an autism diagnosis." (Gabis etal 2021; Lopez-Espejo, etal, 2021). Hypotonia is associated with decreased language development and IQ in autism (Osljeskova etal, 2007; Fillano etal, 2002). Not surprisingly hypotonia is a common symptom in those with autism (Badescu et al, 2016; Oslejskova et al, 2007; Lopez-Espejo et al, 2021; Gabis et al, 2021). Whilst the authors of the aforementioned papers did not come to any conclusion about the reason for vitamin B12 deficiency and hypotonia, clearly in methyl B12 deficiency there is reduced production of creatine, due to the reduced activity of GNMT (Longo etal, 2011; Pacheva etal, 2016; Stöckler et al, 1994; Mercimek-Mahmutoglu et al, 2006; Stockler-Ipsiroglu et al, 2014; Mercimek-Mahmutoglu et al 2014; O'Rourke et al, 2009; Araújo et al, 2005; Lion-François et al, 2006; Mercimek-Mahmutoglu et al, 2009; Leuzzi et al, 2013 Schulze et al, 2006;Verbruggen et al 2007; Morris et al, 2007; Item etal, 2004), and reduced production of CoQ10, both of which would lead to poor muscle tone.
Vitamin B12 Loading of the Foetal Brain
It is known that the majority of vitamin B12 loading of the brain occurs during foetal development where as much as 17% of transplacentally derived vitamin B12 enters the foetal brain. Loading is maximal during the last trimester of foetal life, and continues until the time of birth and thereafter very, very little enters the brain (Roed etal, 2008: Agarwal and Nathani, 2009
). As such foetal loading of the brain is incredibly important for the developing child, and deficiency of vitamin B12 in the mothers has a profound effect on the foetus and new-born child. Deficiency of vitamin B12 in the mothers is also correlated with deficiency of vitamin B12 in the neonate. An alarming rate of vitamin B12 deficiency in pregnant mothers in the UK has recently been reported (Sukumar etal, 206; Knight etal, 2015; Low-Beer etal, 1968), with more that 20% of women deficient as assessed by the haematological definition of deficiency (<150 pmol/L), but a massive 70% being deficient if assessed by metabolic parameters (<250 pmol/L; Sukumar etal, 206; Knight etal, 2015; Low-Beer etal, 1968). It would appear that the rates may have been dropping for some time, because in 1968 (before UK joined the EU), the average B12 levels were much higher at 288 pmol/L (Low-Beer etal, 1968) The rates of deficiency were much higher in India, where 43% were deficient (<150 pmol/L; Krishnaveni etal, 2009). Hopefully this is not a portend of ever increasing rates of autism. Additionally, despite the diagnosis of B12 deficiency, the mothers in the various studies were not treated for B12 deficiency! The incidence of B12 deficiency in pregnancy seems to be very high, with over 50% of woman in Canada being metabolically deficient in the first trimester (Roed etal, 2008). The increase in the adoption of vegan diets will potentially result in a dramatic increase in the rate of both vitamin B12 deficiency and that associated iron deficiency (Lemale etal, 2019), and the associated developmental delay in the upcoming pediatric population.Lower levels of vitamin B12 have been found in the brains of children with autism (Zhang etal, 2016).
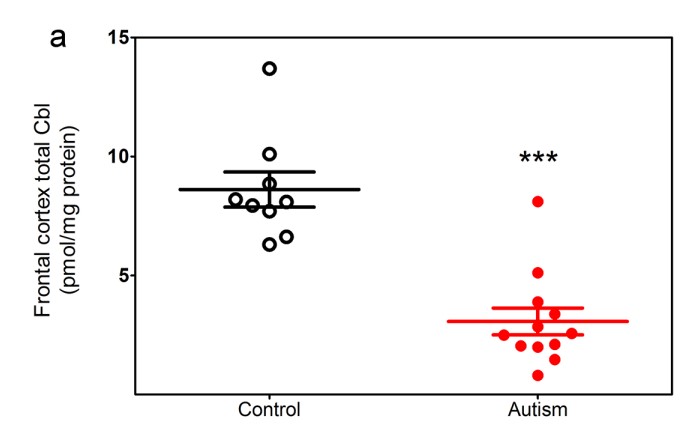
In addition, there is increased homocysteine, and reduced levels of methionine, SAM and lower thiol reducing activity with lower Cysteine, and GSH. Of particular note is the lower level of cystathionine, the initial product of CBS through its reduced action on homocysteine, suggesting a block methylation and in conversion of Hcy to Cystathioinine.

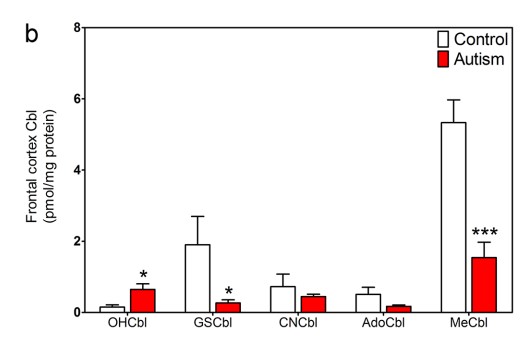
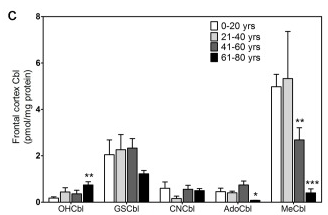
Reduced functional vitamin B12 deficiency is associated with lower activity of the Krebs cycle enzyme, Aconitase, which in turn results in lower energy entering Krebs cycle, higher urinary citrate, and lower Mini Mental score. Lower aconitase activity has been found in the cerebellum and Brodman areas of the brains in those with autism.
Reduced Aconitase activity in the cerebellum and Brodman area of the brain in control and those with autism (Fig from Rose etal, 2012)
Vitamin B12 Deficiency and Neural Tube Defects and Cleft Lip or Palate
Absolute or functional vitamin B12 deficiency in the womb is associated with a higher incidence of Neural Tube Defects, and various oro-facial conditions such as Cleft Lip, Cleft Palate, and Tongue Tie, which may lead to difficulties in the baby breast-feeding (Weekes et al, 1992; Magnus etal, 1986, 1991)
Vitamin B12 Deficiency and Low Birth Weight Babies
Vitamin B12 deficiency in utero has been associated with low birth weight babies. Supplementation of mothers with the combination of active forms MethylCobabalamin and AdenosylCobablamin, significantly increased birthweight (P0.05). Other forms, hydroxyCobablamin and CyanoCobalamin were much less effective (Shah et al, 2017). Supplementation with vitamin B12 forms, especially combination of active forms of cobalamins: MeCbl+AdCbl significantly increased birth weights (p<0.05). Absolute or functional vitamin B12 deficiency in the womb is associated with a higher incidence of Neural Tube Defects, and various oro-facial conditions such as Cleft Lip, Cleft Palate, and Tongue Tie, which may lead to difficulties in the baby breast-feeding (Weekes et al, 1992; Magnus etal, 1986, 1991)
Vitamin B12 Deficiency and Developmental Delay
For over 60 years it has been known that Vitamin B12 sufficiency is crucial for the development of myelination of the central nervous system, and poor vitamin B12 status is linked to poor growth and neurodevelopment (Gutierrez-Diaz, 1959; Schrimshaw etal, 1959; Agrawal and Nathani 2009; Sheng etal, 2019), neural tube defects (Lucke etal 2007), and retardation of myelination in the brain (Lovblad etal, 1997; Horstmann etal, 2003), and lower brain volume (Black 2008). Vitamin B12 deficiency is associated with severe brain atrophy with signs of retarded myelination, with the frontal and temporal lobes being the most severely affected (Lövblad et al,1997). The frontal lobes are involved in motor functions, problem solving, memory, language, judgement, impulse control, spontaneity and social and sexual behaviour. The temporal lobes are involved in the formation of long term memory, recognizing faces, and interpreting body language, it aids in the production of speech, remembering the names of objects, and recognition of language. These are the levels of highest creatine usage with creatine having a role in a range of cognitive functions, including learning, memory, attention, speech and language, and possibly emotion. Thus, vitamin B12 deficiency in the mothers, which is later seen in the children, would be expected to have adverse outcomes. Further, maternal vitamin B12 status early in gestation (28 weeks) has been positively associated with child's subsequent mental and social development quotients, as measured at 2 years (Strand etal 2018). Vitamin B12 concentration in the first 2 years of life was positively correlated with cognitive score (Sheng etal, 2019). Infants aged 12-18 months who have lower B12 levels also present with lower psychomotor and mental development scores compared to those with higher vitamin B12 levels (Obeid etal, 2017). This would "fit" with the critical time for foetal brain loading of the child (Agrawal and Nathany, 2009; Chalouhi etal, 2008), and vitamin B12 and folate deficiency, with the accompanying elevated homocysteine have been associated with altered brain morphology, and cognitive and psychological problems in school-aged children (Ars etal, 2019) . Furthermore, vitamin B12 deficiency, particularly of methyl B12, results in lower production of the methylating agent, S-Adenosylmethionine (SAM). Lower SAM in turn leads to reduced production of creatine (the essential backbone for creatine-phosphate) and ubiquinol (CoQ10), the essential electron transfer molecule in the Electron Transport Chain. A genetic deficiency in creatine production due to lack of activity of the enzyme Guanidinoacetate Methyl Transferase results in autism-like condition (Mercimek-Mahmutoglu S, Salomons, 2015; Stockler-Ipsiroglu et al, 2014). Low CoQ10 levels have been associated with lower cognitive function and intellectual disability in autism (Smolka etal, 2001). Reduced production of SAM also affects the activity of the histamine-neutralizing enzyme, Histamine-N-methyl transferase, and would explain much of the food insensitivity of young children with ASD, due to the presence of histamine in a diverse range of foods. A deficiency in the Adenosyl-form of vitamin B12 has been linked to tiredness, vomiting, weak muscle tone, developmental delay, intellectual disability, and frequent illnesses.
Vitamin B12 Deficiency Overt or Paradoxical?
Functional vitamin B12 deficiency in the neonate can be Overt or Paradoxical. In Overt B12 deficiency, serum vitamin B12 is generally below 200 pmol/L (274 ug/L), and is the result of insufficient intake of vitamin B12 by the mother, due to a vegan or vegetarian diet. Such deficiency is quickly resolved by the injection of vitamin B12. In contrast, in paradoxical B12 deficiency, serum levels of vitamin B12 are generally above 250 pmol/L and the vitamin B12 deficiency is due to a co-deficiency in functional vitamin B2. As such in paradoxical B12 deficiency, the deficiency cannot be resolved simply by injection or high dose administration of vitamin B12, rather the paradoxical vitamin B2 deficiency must be resolved, though the administration of Iodine, Selenium and/or Molybdenum, and then the administration of high dose vitamin B12, either through injection or via topical application of TransdermOilTM Adenosyl/Methyl B12.
Children will not respond to cyanocobalamin.Vitamin B12 and the Production of Melatonin
Melatonin has many important roles in the body, including:
-
Regulation of sleep
-
Differentiation of neuronal stem cells into oligodendrocytes.
-
Maturation of intestinal epithelial cells
-
Maturation and differentiation of the cornea and retina in the eye.
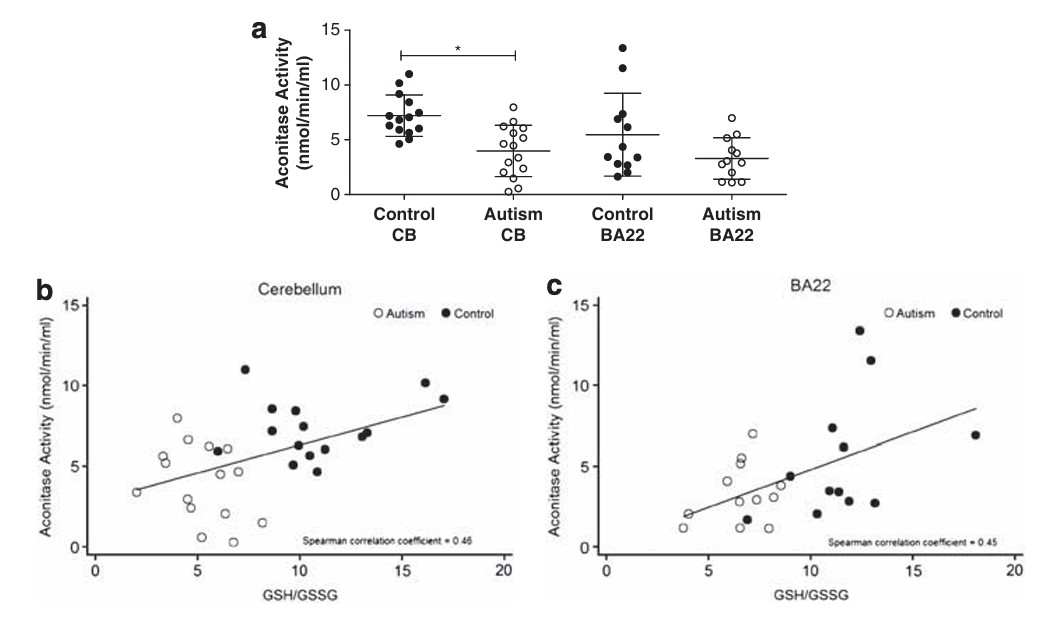
Melatonin, together with vitamin D, stimulates neuronal stem cells to differentiate into oligodendrocytes, which are the cells in the brain that are responsible for myelination of the nerves in the brain. Production of melatonin gradually increases during pregnancy, peaking in the third trimester. After birth, the newborn child initially relies on melatonin in the mother's milk, as it gradually turns on its own production of melatonin, which in neurotypically normal children peaks at around 5 years of age, and starts to decline after puberty. It has been known for over 60 years, that the production of melatonin involves the O-methylation of N-acetyl serotonin, by the action of enzyme hydroxyindole-O-methyl transferase, using S-Adenosylmethionine (SAM), as the methyl donor (Axelrod and Weissbach 1960, Weissbach and Axelrod 1960). As such production of melatonin, ultimately relies on methyl cobalamin as the initial methyl donor for the production of SAM, and so in mothers that are low in vitamin B12, foetal melatonin will be lower, as too will neonatal melatonin, thereby resulting in the delayed myelination typical of ASD. Despite the obvious correlation between low functional vitamin B12 resulting in a reduced ability to produce melatonin, we could find very little evidence that this association has been made in the literature. This is despite countless publications, finding an association between lower melatonin production in the mother, the fetus, or in the neonate, and the severity of symptoms in autism (Wiebe etal, 2018; Yunho etal, 2018; Gagnon and Godbout, 2018; Rossignol and Frye, 2011; 2014, Sanchez-Barcelo et al, 2017; Haidar etal 2016; Abdulamir etal, 2016; Melke etal, 2008). In addition, elevated levels of serotonin, one of the precursors in the pathway to melatonin production, have also been found in children with autism (Jin etal, 2018; Huguet et al, 2016). Further, rather than to measure and address the vitamin B12 deficiency in such children, melatonin is the more common treatment (Blackmer and Feinstein, 2016). There seems to be a general ignorance on the need for B12 for methylation, with study after study and literature review after literature review failing to cite the need for methylB12 sufficiency for the production of sufficient melatonin (Rzepka-Migut and Paprocka, 2020;Jin etal 2018; Gagnon and Godbout 2018; Mantle etal, 2020). Further, the association was still not made in studies showing the elevated melatonin precursor, N-acetylserotonin, and reduced melatonin in ASD (Pagan etal, 2014). Reduced melatonin levels are also associated with sleep disorders, which are common in children with ASD (Goldman et al, 2017; Souders et al, 2016; Geoffray et al, 2016: Cuomo et al, 2017).
Melatonin levels in mothers in the 1st, 2nd, and 3rd Trimester Voiculescu etal, 2014

Melatonin levels during development Grivas and Savvidou, 2007
The final step in production of Melatonin is the methylation of N-Acetyl-Serotonin (NAcSer) by the enzyme HydroxyIndole-O-methyltransferase (HIOMT), which has an absolute requirement for S-Adenosylmethionine (SAM), a product of the methylation cycle (Axelrod and Weissbach 1960, Weissbach and Axelrod 1960).
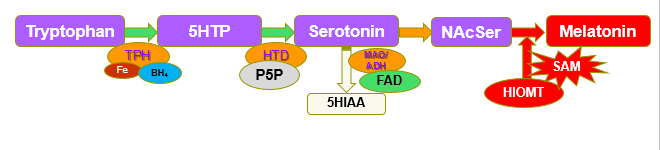
Melatonin synthesis and SAM
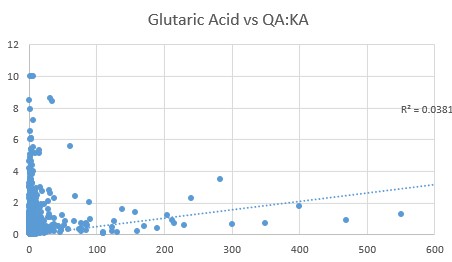
In Methyl B12 deficiency, there is a greatly reduced production of SAM, and breakdown products of tryptophan, Kynurenic acid (KA) and Quinolinic acid (QA), as well as the breakdown product of Serotonin, 5-Hydroxyindoleacetic acid (5HIAA) start to accumulate and can be detected as elevated levels in urine.
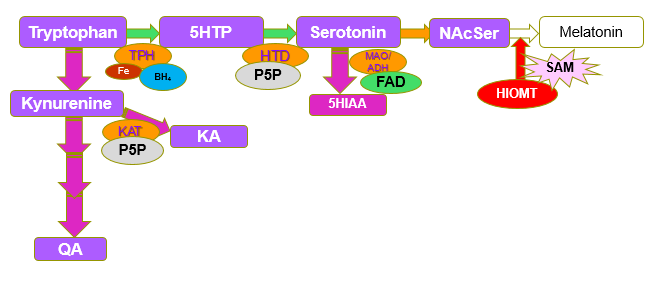
Metabolites increased in SAM deficiency
In functional B2 deficiency due to lack of Iodine and/or Selenium, riboflavin is not converted to FMN and then levels of serotonin and KA are reduced. Symptoms of Iodine/Selenium deficiency are therefore different to Molybdenum deficiency. See Pathway Hence in FAD deficiency, initially there is overproduction of serotonin, which would induce over-secretion of water, and resultant diarrhoea. In Iodine and Selenium deficiency, serotonin is underproduced, which results in irregular digestion and constipation. This can be seen in the graph of 5-hydroxyindoleacetic acid vs glutaric acid. Initially as functional B2 deficiency increases there is a rapid rise in 5HIAA, presumable reflecting increased serotonin production (with resultant side-effects), and later, as vitamin B2 deficiency increases (glutaric acid increases), there is a drop in 5HIAA, as production of serotonin decreases due to lack of conversion of 5HTP due to lack of active B6. Hence, depending upon the extent of glutaric acid deficiency, there may be an over production of serotonin (mod deficiency), whereas in larger deficiency there is an underproduction of serotonin.
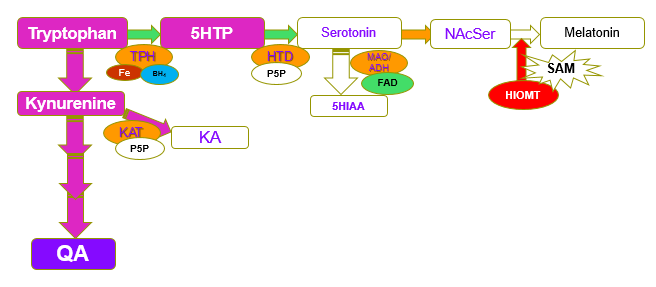
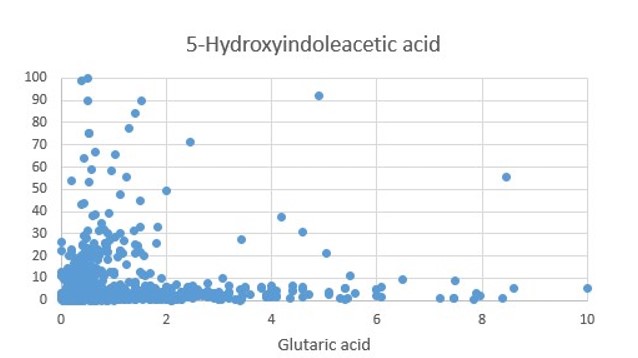
Evidence of the switch to the production of QA can also be seen in the rapid increase in the QA:KA ratio as glutaric acid rises and the almost total absence of 5HIAA as the QA:KA ratio rises.
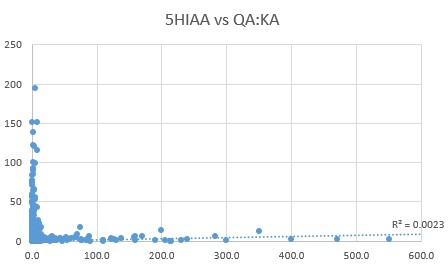
At this point, supplementation with Methyl B12 will not be effective for production of adrenalin, as there is no serotonin precursor .
The typical symptoms of vitamin B12 deficiency in the neonate are very similar to those observed in autism and include megaloblastic anemia, feeding difficulties, developmental delay, difficulty sleeping (Casella etal, 2005; Honzik etal, 2010; Hall 1990), microcephaly (Honzik etal, 2010; Hall 1990), failure to thrive, hypotonia (Aquirre etal, 2019; Casella etal, 2005; Kanra etal, 2005; Chandra etal, 2006; Lucke etal, 2007; Schlapbach etal, 2007; Borkowska etal, 2007; Honzik etal, 2010; Hall 1990), and cerebral atrophy with symptoms of lethargy (Hall 1990; Shevell and Rosenblat 1992), and occasionally seizures (Benbir etal, 2007; Aquirre etal, 2019; Hall 1990), and psycho-motor delay. Seizures may also occur during treatment for B12 deficiency, however, these go away within days or weeks (Benbir etal, 2007) Many of these symptoms can be explained by the critical role that vitamin B12 plays in the production of melatonin, through its role in methylation. Melatonin in turn is critical for the differentiation of neuronal stem cells into myelin-producing oligodendrocytes, potentially explaining the delayed myelination found in children with autism.
Vitamin B12 Deficiency and Creatine deficiency
Over 40% of all methylation within the brain goes to the production of creatine, an essential energy transporter in muscles and brain. As the level of methyl B12 decreases, so too does the formation of creatine. Creatine deficiency has been associated with severe neurodevelopmental delay, intellectual disability, behavioral abnormalities, poorly developed muscle mass and muscle weakness (Stockebrand etal, 2018; Braissant etal, 2011). Creatine deficiency has also been associated with epilepsy and aphasia (difficulty reading, speaking and writing - a common problem in children with autism) (Perna etal, 2016), and with mental retardation, autism, hypotonia, and seizures (Longo etal, 2011). Creatine deficiency has been shown to reduce energy production via the electron transport chain (Nabuurs etal, 2013). Creatine deficiency has also been shown to affect spatial and object learning (Udobi etal, 2019).
Mutations in the enzyme Guanodinoacetate-N-Methyl Transferase (GNMT), which is involved in the formation of creatine, causes mental retardation, hypotonia, autism, and/or behavioural problems, including seizures (Longo etal, 2011; Pacheva etal, 2016; Stöckler et al, 1994; Mercimek-Mahmutoglu et al, 2006; Stockler-Ipsiroglu et al, 2014; Mercimek-Mahmutoglu et al 2014; O'Rourke et al, 2009; Araújo et al, 2005; Lion-François et al, 2006; Mercimek-Mahmutoglu et al, 2009; Leuzzi et al, 2013 Schulze et al, 2006;Verbruggen et al 2007; Morris et al, 2007; Item etal, 2004).
Evidence is accumulating that there may be some benefit in creatine supplementation in children with autism, however, it is not conclusive (Roschel etal, 2021)
Vitamin B12 Deficiency and Elevated pyroglutamate
In methyl vitamin B12 deficiency, there is reduced production of S-Adenosylmethionine (SAM), and the activity fo the enzyme cystathionine beta synthase is reduced, thus leading to reduced transfer of the sulphur from methionine into the sulphation cycle, with a resultant lack of production of Glutathione. The cell tries to drive the reaction Glu-Cys-Gly, but lack of cys, results in activation of the enzyme glutaminyl cylase, and the over-production of pyroglutamic acid. Elevated glutaminyl cyclase activity has been associated with Alzheimer's disease, Huntington's disease, Melanomas, thyroid carcinomas and other conditions, whilst elevated pyroglutamate is common in autism, CFS, paradoxical B12 deficiency, and Parkinson's disease (personal observations). Data suggests that elevate pyroglutamate is the result of functional vitamin B2 deficiency, which in turn leads to functional vitamin B12 deficiency. Unfortunately we have been unable to find any research in which this correlation has been tested. Data presented is from over 1800 subjects.
 , . ,
, . ,
Energetics of Vitamin B12 Deficiency
The higher the vitamin B12 deficiency the lower the energy output is from the electron transport chain - due to lower production of CoQ10, and the lower the energy transfer from the mitochondria into the cytoplasm of the cell, due to reduced creatine production. In addition in severe B12 deficiency, the reduced production of free GSH, leads to lower levels of production of iron-sulphur proteins, such as aconitase, thereby leading to lower energy transfer into the Citric Acid Cycle.
Adenosyl Vitamin B12 Deficiency
A deficiency in the Adenosyl-form of vitamin B12 has been linked to tiredness, vomiting, weak muscle tone, developmental delay, intellectual disability, and frequent illnesses. In functional B2 deficiency, the child has reduced capacity to gain energy from fats, as the reductase is FAD-dependent, or to gain energy from sugar, due to the need of pyruvate decarboxylase for TPP, lipoate and FAD. Hence the body turns to the metabolism of protein for energy. The break-down of proteins results in increased levels of the 9 essential amino acids lysine, tyrosine, phenylalanine, tryptophan, methionine, and the branched chain amino acids leucine, isoleucine, and valine, which is common in autism (Saleem et al, 2020). Of these lysine, tyrosine, phenylalanine and tryptophan cannot be processed for energy as their break-down products enter the glycolysis pathway and so cannot be used, thus energy must be obtained from methionine, and the branched chain amino acids (BCA acids). Processing of the later requires MMA-CoA mutase an Adenosyl-B12 dependent enzyme. In Adenosyl-B12 deficiency, levels of urinary methyl malonic acid are elevated. Elevated BCA acids are found in autism (Gao et al, 2024)
Other markers of Adenosyl B12 deficiency include ethyl malonic acid, and methyl succinic acid. Methylsuccinate is a by-product of the metabolism of methionine and threonine. Ethylmalonic acid and methylsuccinic acid are altered metabolites of isoleucine (Nowaczyk et al, 1998). Elevated ethylmalonicacid and methylsuccinic acid have been associated with developmental delay, hypotonia, and vascular instability associated with lactic acidemia (Nowaczyk et al, 1998). Functional vitamin B2 deficiency, also results in the catabolism of hydroxyproline, leading to elevated oxalate, pyruvate, hippuric acid, glycolate, and glyoxylate. Elevated levels of MMA, EMA, MSA, oxalate, hippuric acid, glycolate and glyoxylate are common in autism.
Vitamin B12 Deficiency in Vegetarian Mothers
Studies have shown that the incidence of vitamin B12 in vegetarian mothers can be as high as 62%, with deficiency of 25-86% among the children of vegetarian mothers (Pawlak etal 2013). Children born of vegan, vegetarian, and ovo-lacto-vegetarian mothers often have moderate to severe vitamin B12 deficiency (and accompanying iron deficiency)
, and such deficiencies have been associated with delayed myelination, weight loss, and reduction of motor skills, delayed development, neuro-regression, regression of psychomotor development, growth retardation, neuropathy (Renault etal, 1999) brain atrophy and apathy (Davis and Melina 2014; Kanra etal, 2005; Stollhoff and Schulte 1987; Von Schenck et al, 1997; Daphna etal, 2008: Chalouhi etal, 2008). Many of these conditions persist through later life (von Schenck etal, 1997), and even with supplementation after birth, children can still show apathy, muscular dystonia, abnormal movements and language delay (Smolka etal 2001).Other symptoms can be hypotonia, involuntary movements, and infantile tremor syndrome (Goroya etal, 2015). Despite these deficiencies being well documented, for more than 30 years, many vegetarian and vegan mothers do not supplement before, during or after pregnancy, nor do their health professionals check them for deficiency.Accompanying the vitamin B12 deficiency of the vegan and vegetarian diets are deficiencies in protein, calcium, iron, zinc, and omega-3 fatty acids (97-98-99), so much so that the German Nutrition Society does NOT recommend such diets during pregnancy, lactation, and childhood (99).
Maternal serum B12 levels are closely correlated with the vitamin B12 levels in the mother's milk. In the years 2009 to 2017, there was an increase in the rate of veganism in the US from 0.1% to 6%, and in increase in the rate of autism from 1:200 to 1:35 over the same period. Similarly rates of veganism in Australia in 2021 now reaching 12.1%, paralleling the rise in autism in the country, whilst it is claimed that 13 million Brits will be meat-free by the end of 2021. Small wonder that the rates of autism have risen dramatically.
Vitamin B12
deficiency, due to its involvement in methylation, leads to reduced methylation
in autism with reduced production of SAM, a lower SAM:SAH ratio, and
hypomethylation of DNA (James etal, 2009; Indika etal, 2021; Guo etal, 2020;
James et al, 2004), and lower production of glutathione (Lu,
2009)
Vitamin B12 deficiency and Reduced
Methylation in Autism
Vitamin B12 and the Development of Speech
Myelination of Brocca's region in the brain precedes the development of speech, and as such delayed myelination would be expected to cause the delay in speech which is so characteristic of many children with autism (Conrad et al, 2021; Wang et al, 2020; Brauer et al, 2010; Su et al, 2008; Hahn et al, 2016; Mohr et al, 2020). The density of myelination in the area surrounding Broca's region predicts the "grammar learning success of children" (Floel et al, 2009). Studies have shown that increasing the rate of methyl B12 cycling through the addition of excess folinic acid, improves the development of speech (Frye et al, 2016). The reduced activity of aconitase in Brodman's region, can account for much of the delay in the development of speech (Rose etal, 2012)
Vitamin B12 deficiency and myelination of the brain
As mentioned above, vitamin D and vitamin B12 work together in stimulating myelination of nerves in the brain. Insufficient myelination of the brains has been found in post-mortem of brains of people with autism (Deoni etal, 2015). Within the autistic individuals, the lower the myelination the lower worse the social interaction skills.
Vitamin B12 deficiency and Optic Neuropathy
Vitamin B12 deficiency has been associated with partially reversible optic neuropathy in some children with autism (Pineles etal, 2010), and potentially could explain the increased risk of optic neuropathy in children with autism (Chang etal, 2020;
Vitamin B12 Deficiency and Sleep
Melatonin, which is a product of methylation is an essential hormone involved in regulation of sleep.
Approximately two thirds of children with ASD have sleeping difficulties (Souders etal, 2017; Ming and Wlaters, 2009), which is in line with functional B12 deficiency in autism. Despite the fact that it has been known for over 40 years that there is a requirement for Methylation in the production of melatonin via the enzyme HIOMT (Pevet etal, 1980), treatment for poor sleep in ASD by correction of functional B12 deficiency is generally not attempted (Souders etal, 2017; Yuge etal, 2020; Malow, 2004; McDonagh etal, 2019; Lázár etal, 2008; Accardo and Marlow, 2014; Johnson and Zarrinnegar, 2021).Vitamin B12 deficiency and Epilepsy
Vitamin B12 deficiency is common in those with epilepsy, either as a cause or as a result of treatment with anti-epileptic drugs (Youness, etal, 2020; Li, etal, 2015; Dinç, and Schulte, 2018; Silva, etal, 2019; Glaser, etal, 2015; Matsumoto, etal, 2009; Diaz-Arrastia 2000; Meena, etal, 2018; Ma, etal, 2011; Aslan, etal, 2008; Korenke, etal, 2004).
Vitamin B12 deficiency and Nitrous oxide and anaesthetics.
Use of Nitrous oxide either as an anaesthetic or though inhalation from a "Nang" can have disastrous affects on the function of vitamin B12. During the methylation reaction of MethylCo(III)B12 + Homocysteine, the product, Co(I)B12 + Methionine is formed. In the absence of 5MTHF, free Co(I)B12 can readily reacts with nitrous oxide to form NO-Co(III)B12, which is inactive, yet will “clog up” methylation by Methionine synthase, and irreversibly inactivate the enzyme, hence explaining the toxicity of Nitrous oxide..
Higher levels of Co(I)B12 are present in functional B2 deficiency, due to lack of activity of MTHFR, particularly with those mutations in the MTHFR protein , or in those with a diet low in folate, thereby making those individuals more susceptible to the action of Nitrous oxide. The inactive NO-Co(III)B12 would be indistinguishable from inactive Co(II) B12, and when measured in the current total serum B12 and the inappropriately named active B12 tests, as they do not distinguish which analogue of cobalamin is being measured, cyanocobalamin, hydroxycobalamin, methylcobalamin, adenosylcobalamin, Co(II)cobalamin, Co(I)cobalamin, glutathionyl-Co(III)cobalamin or NO-Co(III)cobalamin, to name but a few. The extent of damage that nitrous can do to the nervous system can be gleaned from those who use Nangs, and their devastating neurological consequences. Reports of side-effects include “subacute-onset, progressive distal lower limb sensory symptoms and unsteadiness”, “subacute combined degeneration of the cord”” ataxia and progressive paresis”, depression, development of diseases of the brain, spine and nerves. The severity of these reactions has led the UK government to consider criminalizing the use of Nitrous Oxide.
Nitrous oxide was commonly used as an anaesthetic gas, yet as long ago as 1956 (Lassen et al, 1956) it was realized that it the activity of vitamin B12 was destroyed by nitrous oxide and could cause megaloblastic anemia. In 1968, Banks and co-workers demonstrated that nitrous oxide could react with the cobalt in vitamin B12 and lead to the inactive NO-CoB12 complex. The destruction of the activity of vitamin B12 is dependent upon the time and dose of administration of nitrous, with over 50% of individuals producing signs of megaloblastic depression of bone marrow function (Nunn and Chanarin, 1978). As early as 1978 (Amess et al, 1987) the use of nitrous oxide for anaesthesia was found to be contra-indicated, yet to this day it is still used, and many individuals report signs of B12 deficiency following use. Unbelievably, despite numerous publications showing poor outcomes of nitrous oxide use in pregnancy, and several demonstrating an association between nitrous and autism, and over 200 publications, demonstrating inactivation of vitamin B12 with subsequent sequelae, clinicains in the US, UK and Australia claim "“ Initiation and management of nitrous oxide by registered nurses is a safe and cost-effective option for labor pain.”. (See PDF). One of the problems with Nitrous inactivation of vitamin B12 activity is that the levels of B12 in serum still remain high, yet paradoxically the B12 is inactive - as per the discussion on paradoxical vitamin B12 deficiency. Unbelievably, nitrous oxide is still used as an anaesthetic to this day in the USA and Australia, both on mothers during pregnancy, and also on young children. Evidence suggests that this alone is responsible for many cases of autism (Xin et al, 2024). It has been known for over 40 years that the use of nitrous oxide in anaesthesia (laughing gas) or in recreational abuse, can cause vitamin B12 deficiency (Shah and Murphy, 2019: Tani etal, 2019; Oussalah etal, 2019; Chi, 2018; Stockton etal, 2017; Massey etal, 2016: Garakani etal, 2014; Safari etal, 2013; Chiang etal, 2013; Krajewski etal, 2007; Cohen etal, 2007; Jameson etal, 1999; Smith, 2001: Deleu etal, 2001; Mayall, 1999; Horne and Holloway, 1997: Kinsella and Green 1995; Carmel etal, 1993; Koblin etal,1990; O'Leary etal, 1985; van der Westhuyzen and Metz, 1984; 1982; Lumb etal, 1982; Kondo etal, 1981: Seteinberg etal, 1981; McKenna etal, 1980; Linnell etal, 1978; Deacon etal, 1978). Post surgical complications of the use of Nitrous include peripheral neuropathy (Neuveu etal, 2019: Egan, 2018: Kaski etal, 2017; Richardson 2010), metabolic encephalopathy (Vive etal, 2019), myeloneuropathy (Edigin etal, 2019; Friedlander and Davies, 2018; Alt etal, 2011; Waklawik etal, 2003; Sesso etal, 1999: Nestor and Stark, 1996), neuropathy (Gullestrup etal, 2019; Conaerts etal, 2017:Middleton and Roffers, 2018), pancytopenia (Norris and Mallia, 2019), Myopathy (Williamson etal, 2019), myelopathy (Dong etal, 2019; Mancke etal, 2016; Probasco etal, 2011: Hathout and El-Saden, 2011; Pema et al, 1998), severe neuropsychiatric symptoms (Lundin etal, 2019), combined degeneration of the spinal chord (Lan etal, 2019; Patel etal, 2018; Anderson etal, 2018; Antonucci, 2018; Keddie etal, 2018; El-sadawi etal, 2018; Yuan etal 2017: Buizert etal, 2017; Chen and Huang, 2016; Pugliese etal, 2015: Chaugny etal, 2014; Cheng etal, 2013; Lin etal, 2011; Wijesekera, etal, 2009; Renaud etal, 2009: Wu etal, 2007; Ahn and Brown, 2005 Ilniczky etal, 2003: Beltramello etal, 1998: Rosener and DIchgans, 1996), neurotoxicity (Johnsonn etal, 2018), neuronopathy (Morris etal, 2015), polyneuropathy (Alarcia etal, 1999), psychosis (Sethi etal, 2006), dementia (El Otmani etal, 2007), ataxia (Miller etal, 2004), megaloblastic anemia (Barbosa etal, 2000), neurological impairment (McNeeely etal, 2000), neurologic decompensation (Felmet etal, 2000), neurologic degeneration (Flippo and Holder, 1993), spastic paraparesis (Lee etal, 1999). Curiously, Nitrous is still recommended by the American Association of Anesthesiologists, NSW Department of Health, and the Association of Anesthesiologists, the New Zealand College of Midwives.. In fact, several countries with high standards of healthcare, such as Canada, Sweden, Australia, Finland, and the United Kingdom, use a blend of 50% oxygen and 50% nitrous oxide to treat pain during labor.They do, though, express concerns about the potential effect on Global warming, which is of greater concern that the effect on the neonatal brain!! The rational appears to be due to the replacement of epidural medication, with its risk on the spine, with the nitrous oxide. This attitude typifies the medical profession, treat the problem now, worry about the side effects later. We have contacted numerous hospitals, the Royal Children's Hospital Melbourne, Mayo Clinic Kopabirth, NZ College of Midwives, midwife associations, The America Pregnancy Association, Queensland Government, Doctors for the Environment and anaesthesiologists expressing our concerns yet not one has "returned our call". Atrocious!! Interestingly, the increase in the use of Nitrous from around 1% of births in 1980 to now 35=45% of births in 2024, has paralleled the rise in the rate of autism from <0.1% to now ~ 3%.
Vitamin B12 deficiency and Histamine Intolerance
It has recently been found that there is a critical role for histamine in the brain in cognition, sleep, and other behaviours. Control of histamine stimulation in the brain occurs via inactivation by the enzyme Histamine-N-Methyl Transferase (HNMT), which is known to be over-expressed in the brain. In vitamin B12 deficiency, lack of production of the methylating agent, SAM, would lead to a reduced ability to control the effects of histamine in the brain.
Markers associated with Vitamin B12
SAM:SAH ratio As vitamin B12 deficiency increases lack of methyl transferase activity leads to elevations in Homocysteine, and a decrease in the ratio of SAM:SAH
GSH:GSSG ratio. Reduced methylation causes a reduction in the transfer of the sulphur from homocysteine into the sulphation cycle, leading to lower intracellular cysteine, and reduced production of glutathione. Lack of cysteine then causes an increase in Pyroglutamic acid, one of the surrogate markers for vitamin B12 deficiency. Reduced GSH works in combination with thiosulfate sulphur transferase in the formation of SeCystRNA, and the efficacy of the reaction drops in functional B12 deficiency. In addition levels of toxic intracellular sulphite increase (ASD 107 nmol/ml, NT 2.1 nmol/ml) as well as thiosulfate (ASD 131 nmol/ml, NT 19 nmol/ml) (Kruithof et al, 2020). This can then result in a metabolic spiral, as lack of production of SeCystRNA, will reduce the production of Selenoproteins, such as the deiodinases that are responsible for conversion of T4 to T3. This in turn leads to lower production of ribofavin kinase, with a reduced activity of MTHFR and MTRR, which are critical for maintaining the activity of MethylB12.
Determination of vitamin B12 Deficiency
Simplistically one would assume that simply measuring vitamin B12 levels in serum would determine if a person was sufficient or insufficient, and to a large extent this is what is done. Most Pathology labs simply measure the amount of B12 in serum and using an arbitrary cut-off value (generally 150 pmol/L) assign values above this as being sufficient. Unfortunately it is nowhere near that simple. Even in common dietary insufficiency, signs of biochemical deficiency of vitamin B12 can be observed when vitamin B12 levels drop below 250 pmol/L.
Measurement of biochemical deficiency has uncovered a huge range of serum B12 levels even as high as 2000 pmol/L in which biochemical deficiency of vitamin B12 can be measured. This, then is paradoxical and the term "Paradoxical vitamin B12 deficiency" has been used to describe this condition. It appears that in "paradoxical B12 deficiency", the form of B12 that is in serum is an inactive form of B12 (most likely to be Co(II)B12). If this form of B12 was present in the mother during pregnancy it would be this form of B12 (the inactive Co(II)B12) that would have stocked the brain, with the result that the child would be born with what seems to be adequate vitamin B12 levels, however, the child would be functionally deficient in vitamin B12. Further, the B12 in breast milk from the mother would also be inactive. Paradoxical B12 deficiency is common in children with ASD (Hope etal, 2020). Studies by Dr Russell-Jones have shown that every child with ASD was functionally deficient in vitamin B12, with the majority also having Paradoxical B12 deficiency.
Thus, the only way to tell if the vitamin B12 in serum is active or inactive is to measure metabolic by-products of B12 metabolism and see if they are raised. The two most commonly raised markers in vitamin B12 deficiency are homocysteine and methyl malonic acid (MMA). There are a number of others that are readily identified if an assessment of urinary Organic Acids is performed. Interpretation of such data should though only be attempted by those sufficiently trained in such assessment, which the general medical profession are not.
Resolving Vitamin B12 Deficiency in Pregnant mothers
Mothers should ensure vitamin B12 sufficiency before they are pregnant, however, if this is not possible, urinary Organic Acids Testing should be carried out to establish sufficiency, and cases of deficiency mothers should supplement not only with vitamin B12, but also with Iodine, Selenium, Molybdenum and vitamin B2 if there is reason to believe that these may also be deficient. Warning signs in the mothers can be fatigue, obesity, gestational diabetes, insufficient dietary intake such as occurs in vegetarian or vegan diets. Correcting of deficiency cannot be achieved by large oral doses of vitamin B12 due to both the very limited uptake of vitamin B12 from the gut, as well as the extensive denaturation of the majority of the orally administered dose of vitamin B12, by gastric acid. Instead vitamin B12 should be given by injection or via the TransdermoilTM delivery route. Any person on antidepressant medication going into or during pregnancy should suspect vitamin B12 or iron deficiency, and get checked via OAT. Studies have shown that maternal vitamin B12 supplementation during pregnancy was associated with higher expressive language scores in children at 30 months. Functional vitamin B12 deficiency during pregnancy, as defined by elevated homocysteine in the mothers, had negative associations with expressive language and gross motor domains (Thomas et al, 2018). Care must be taken during supplementation that there are not other confounding deficiencies, such as Iodine, iron and vitamin D deficiencies, as each of these also causes developmental delay, and so if these are not fixed, then delay can still occur, such as occurred in the study by Chandyo and co-workers (2023).
Vitamin B12 deficiency and depression in mothers
Indicative signs of vitamin B12 deficiency may be the use of anti-depressants in the mothers during pregnancy. Use of anti-depressants, and also depression in the mothers has been associated with an increased risk of having a child with autism. Vitamin B12 deficiency should be suspected in mothers who become pregnant whilst on antidepressants such as SSRIs or benzodiazepines, or who start to use these drugs during pregnancy "that use of ADs during the second and /or third trimester is associated with an 87% increased risk of having a child with ASD" (Boukhris et al, 2016; Mezzacappa et al, 2017; Pedersen, 2015; Sujan et al, 2017; Brown et al, 2017; Becker et al, 2016; Morales et al, 2018; Andrade 2017; Rai et al 2017, 2013; Viktorin et al 2017; Yamamoto-Sasaki et al,, 2019; Hagberg etal, 2018; Andrade et al, 2017; Zhou et al, 2018).. Interestingly the second most common symptom in those who are vitamin B12 deficient is depression
Vitamin B2 and Vitamin B12 Co-Deficiencies in Autism
Whilst previously there are many examples of developmental delay just due to vitamin B12 deficiency, nowadays there almost always exists a co-deficiency of both functional Vitamin B2 and vitamin B12. Due to the absolute dependence of the function of vitamin B12 and active vitamin B2, as FMN and FAD, the deficiency of vitamin B2 MUST be addressed first before substantial progress can be made with fixing the vitamin B12 deficiency. Curiously the absolute need for vitamin B2 for vitamin B12 cycling appears to have been missed by the majority of authors and reviewers in the field (Zaric etal, 2019)
Resolving Vitamin B12 Deficiency in Neonates
Once overt vitamin B12 deficiency has been demonstrated in the neonate, in which serum vitamin B12 is lower than 250 pmol/liter, this should be addressed, either by injection of mixed Adenosyl/Methyl B12, or by topical application of teh mixed Adenosyl/methyl B12 oils. Resolution of the deficiency may take some time, which is related to how long the child has been deficient. Resolution of vitamin B12 deficiency should be monitored by serum B12 levels, homocysteine, MMA or via Organic Acids testing. During resolution changes in temperament are common, and may be accompanied by anxiety, anger, or depression. (see https://b12oils.com/receptors.htm Iron deficiency often accompanies the vitamin B12 deficiency, and this should be addressed once the vitamin B12 deficiency has been resolved.
Resolving Vitamin B12 Deficiency in Autism
Vitamin B12 deficiency has been shown to occur in all children with ASD and this needs to be addressed if the child is going to have any chance of normal development. Several studies on children who were vitamin B12 deficient have shown significant increase in growth and cognitive scores when supplemented with vitamin B12 (Sheng etal, 2019; Strand etal, 2015). Given that co-deficiency in functional vitamin B2 is universal in autistic children this deficiency must be fixed first, and then the active forms of vitamin B12, adenosyl B12 and methyl B12 must be given either by injection or via the TransdermoilTM delivery route
. NO oral formulation of vitamin B12 has ever been shown to resolve symptoms in ASD, dementia, or to improve cognition (Moore etal, 2012). The importance of functional vitamin B2 for maintaining vitamin B12 activity, cannot be over-stated, yet review after review on the cycling of vitamin B12, omits this important influence of vitamin B2 on B12 cycling (Frye etal, 2020)Other signs of Vitamin B12 Deficiency in Neonates
Other signs of vitamin B12 deficiency in the neonate include megalobastic anaemia, feeding difficulties (difficulties in suckling), developmental delay, microcephaly, hyptonia, lethargy, irritability, involuntary movements, seizures and cerebral atrophy" (Benbir etal, 2007).
Other signs of Vitamin B12 Deficiency in Adults
There are many neuropsychiatric symptoms associated with functional vitamin B12 deficiency, including, depression, anxiety, psychosies, dementia, delirium, apathy, agitation, impraired concentration, insomnia, persecutory delusions, auditory and visual hallucinations, schizophrenia, and disorganized thought processes.
Associated Deficiencies in Autism
The majority of studies looking at vitamin B12 deficiency in children and in autism have now addressed the likely co-deficiency of iron, however, one could assume that a diet low in vitamin B12 would also be a diet low in iron. Every child that we have data for who has autism is also deficient in active vitamin B2 (FMN and FAD) and is deficient in active vitamin B12 (Adenosyl and Methyl B12), these deficiencies also have to be addressed or the child will not progress developmentally. Accompanying these deficiencies, deficiencies of Iodine, Selenium and/or Molybdenum are very common.
Resolving Vitamin B12 Deficiency in the Brain
Transport of vitamin B12 into the brain happens primarily during the last trimester of pregnancy. Once this has occurred, the brain becomes almost recalcitrant to further uptake of vitamin B12, and seems to have to survive on what was in the brain at the time of birth. This can be seen in levels of vitamin B12 detected in the brains of subjects with normal serum B12 levels as they age (Zhang et al, 2016). Of particularly note is the huge drop in both Methyl and Adenosyl B12 in the Frontal Cortex in those over 61..
Attempts to resolve this deficiency through intravenous administration are hindered by the very limited amount of vitamin B12 taken into the brain following even intravenous administration, as can be seen in numerous imaging studies.
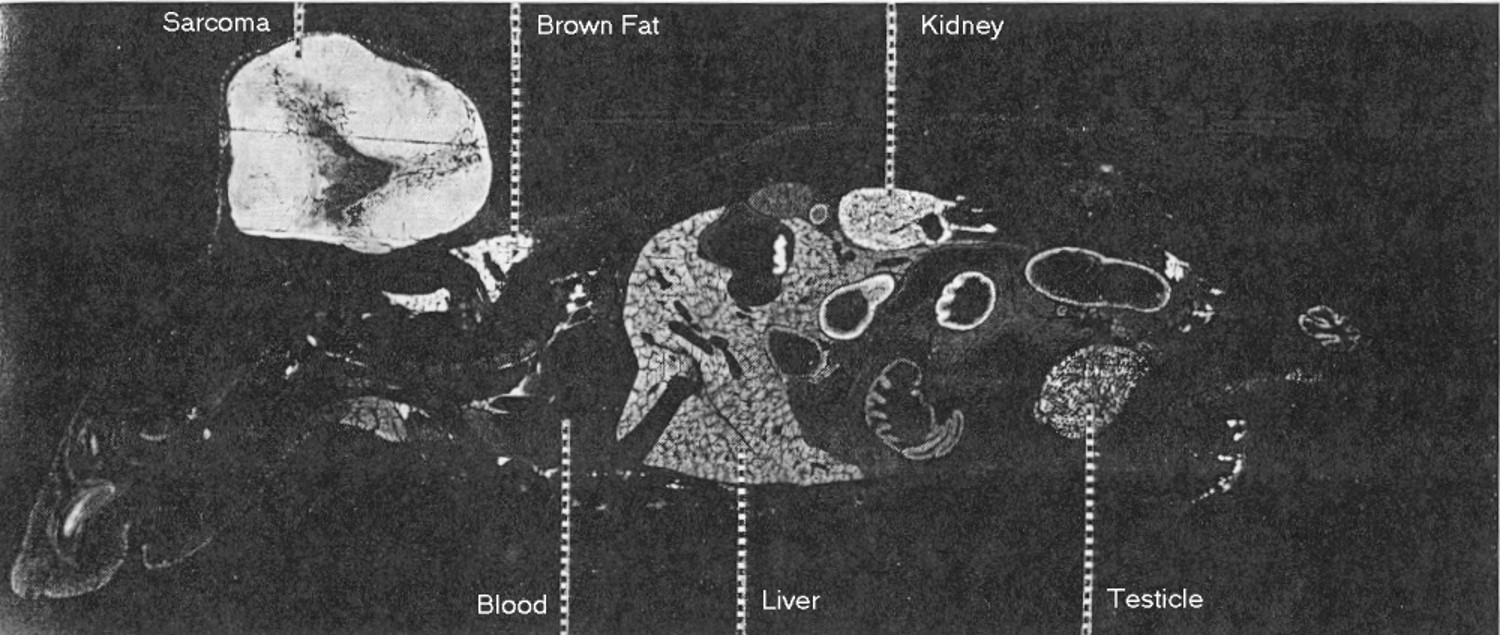
As can be seen in the study by Flodh (1967), the brain of the mouse seems to have virtually no uptake of 131-I-cobalamin.
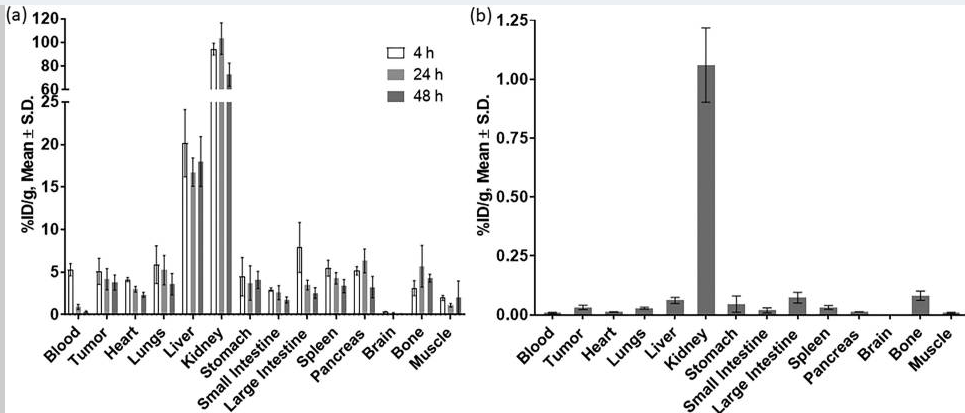
Calculation of 89Zr-Cobalamin PET Tracer (Workinger, et al, 2017), confirmed these findings, and showed almost no detectable uptake into the brain.
The corollary to this is that if, the brain is loaded with "dud" B12 in utero, or if the brain is exposed to vitamin B12 modifying agents such as Nitrous Oxide, it will be almost impossible to displace the alterred vitamin B12.
Copyright.
The descriptions and findings on vitamin B12 and autism, is the property of B12 Oils Pty Ltd. Reproduction in whole or in part constitutes an infringement in the Copyright law. Copyright infringement carries serious penalties.
References
-
Black 2011 Effects of vitamin B12 and folate deficiency on brain development in children
PMC3137939
-
Acıpayam C, Güneş H, Güngör O, İpek S, Sarışık N, Demir NŞ. Cerebral atrophy in 21 hypotonic infants with severe vitamin B12 deficiency. J Paediatr Child Health. 2020 May;56(5):751-756. doi: 10.1111/jpc.14733. Epub 2019 Dec 23. PMID: 31868292.
-
Jain etal 2015 Vitamin B12 deficiency in children: a treatable cause of developmental delay
24453156
-
Rasmussen etal, 2001 Vitamin B12 deficiency in children and adolescents
S0022
-
Hasbaoui BE, Mebrouk N, Saghir S, Yajouri AE, Abilkassem R, Agadr A. Vitamin B12 deficiency: case report and review of literature. Pan Afr Med J. 2021 Mar 4;38:237. doi: 10.11604/pamj.2021.38.237.20967. PMID: 34046142; PMCID: PMC8140678.
-
Bousselamti A, El Hasbaoui B, Echahdi H, Krouile Y. Psychomotor regression due to vitamin B12 deficiency. Pan Afr Med J. 2018 Jun 20;30:152. doi: 10.11604/pamj.2018.30.152.12046. PMID: 30374398; PMCID: PMC6201603
-
-
Casella EB, Valente M, de Navarro JM, Kok F. Vitamin B12 deficiency in infancy as a cause of developmental regression. Brain Dev. 2005 Dec;27(8):592-4. doi: 10.1016/j.braindev.2005.02.005. PMID: 16310594
-
Serin HM, Arslan EA. Neurological symptoms of vitamin B12 deficiency: analysis of pediatric patients. Acta Clin Croat. 2019 Jun;58(2):295-302. doi: 10.20471/acc.2019.58.02.13. PMID: 31819326; PMCID: PMC6884369
-
Bicakci Z. Growth retardation, general hypotonia, and loss of acquired neuromotor skills in the infants of mothers with cobalamin deficiency and the possible role of succinyl-CoA and glycine in the pathogenesis. Medicine (Baltimore). 2015 Mar;94(9):e584. doi: 10.1097/MD.0000000000000584. PMID: 25738478; PMCID: PMC4553967.
-
Serin HM, Kara AO, Oğuz B. West syndrome due to vitamin B12 deficiency. Turk Pediatri Ars. 2015 Dec 1;50(4):251-3. doi: 10.5152/TurkPediatriArs.2015.1492. PMID: 26884697; PMCID: PMC4743870.
-
Taskesen M, Yaramis A, Pirinccioglu AG, Ekici F. Cranial magnetic resonance imaging findings of nutritional vitamin B12 deficiency in 15 hypotonic infants. Eur J Paediatr Neurol. 2012 May;16(3):266-70. doi: 10.1016/j.ejpn.2011.08.005. Epub 2011 Sep 7. PMID: 21903432.
-
Hall CA. Function of vitamin B12 in the central nervous system as revealed by congenital defects. Am J Hematol. 1990 Jun;34(2):121-7. doi: 10.1002/ajh.2830340208. PMID: 1692663.
-
Lücke T, Korenke GC, Poggenburg I, Bentele KH, Das AM, Hartmann H. Mütterlicher Vitamin-B12-Mangel: Ursache neurologischer Symptomatik im Säuglingsalter [Maternal vitamin B12 deficiency: cause for neurological symptoms in infancy]. Z Geburtshilfe Neonatol. 2007 Aug;211(4):157-61. German. doi: 10.1055/s-2007-981249. PMID: 17729202
-
Casella EB, Valente M, de Navarro JM, Kok F. Vitamin B12 deficiency in infancy as a cause of developmental regression. Brain Dev. 2005 Dec;27(8):592-4. doi: 10.1016/j.braindev.2005.02.005. PMID: 16310594
-
Vieira D, Florindo C, Tavares de Almeida I, Macário MC. Adult-onset methylenetetrahydrofolate reductase deficiency. BMJ Case Rep. 2020 Mar 10;13(3):e232241. doi: 10.1136/bcr-2019-232241. PMID: 32161077; PMCID: PMC7066602.
-
Lövblad K, Ramelli G, Remonda L, Nirkko AC, Ozdoba C, Schroth G. Retardation of myelination due to dietary vitamin B12 deficiency: cranial MRI findings. Pediatr Radiol. 1997 Feb;27(2):155-8. doi: 10.1007/s002470050090. PMID: 9028851
-
Kose E, Besci O, Gudeloglu E, Suncak S, Oymak Y, Ozen S, Isguder R. Transcobalamin II deficiency in twins with a novel variant in the TCN2 gene: case report and review of literature. J Pediatr Endocrinol Metab. 2020 Nov 26;33(11):1487-1499. doi: 10.1515/jpem-2020-0096. PMID: 32841161.
-
Tosun A, Aral YZ, Çeçen E, Aydoğdu A, Çetinkaya Çakmak B. Involuntary movement in infants during vitamin B12 treatment. Turk J Haematol. 2011 Dec 5;28(4):317-22. English. doi: 10.5152/tjh.2011.18. PMID: 27264590
-
Kamoun F, Guirat R, Megdich F, Ben Ameur S, Kallel C, Hachicha M. Frequent Infections, Hypotonia, and Anemia in a Breastfed Infant. J Pediatr Hematol Oncol. 2017 Mar;39(2):141-142. doi: 10.1097/MPH.0000000000000725. PMID: 28060111.
-
Wagnon J, Cagnard B, Bridoux-Henno L, Tourtelier Y, Grall JY, Dabadie A. Allaitement maternel et végétalisme [Breastfeeding and vegan diet]. J Gynecol Obstet Biol Reprod (Paris). 2005 Oct;34(6):610-2. French. doi: 10.1016/s0368-2315(05)82888-1. PMID: 16208206.
-
Borkowska A, Plata-Nazar K, Łuczak G, Matheisel A. Niedobór witaminy B12 u rocznego dziecka karmionego wyłacznie piersia [Vitamin B12 deficiency in a one-year-old, exclusively breast fed child]. Med Wieku Rozwoj. 2007 Oct-Dec;11(4):435-8. Polish. PMID: 18605198.
-
Ma X, Zhang Y, Yang Y, Liu X, Yang Z, Bao X, Qin J, Wu X. Epilepsy in children with methylmalonic acidemia: electroclinical features and prognosis. Brain Dev. 2011 Oct;33(9):790-5. doi: 10.1016/j.braindev.2011.06.001. Epub 2011 Jul 20. PMID: 21764232.
-
Sukumar etal, 2016 Vitamin B12 status among pregnant women in the UK and its association with obesity and gestational diabetes. PMID 27916927
-
Knight etal 2015 Lower circulating B12 is associated with higher obesity and insulin resistance during pregnancy in a non-diabetic white British Population. PMID
-
Weekes, E.W.; Tamura, T.; Davis, R.O.; Birch, R.; Vaughn, W.H.; Franklin, J.C.; Barganier, C.; Cosper, P.; Finley, S.C.; Finley, W.H. Nutrient levels in amniotic fluid from women with normal and neural tube defect pregnancies. Biol. Neonate 1992, 61, 226–231. 55.
-
Magnus, P.; Magnus, E.M.; Berg, K. Increased levels of apo-transcobalamins I and II in amniotic fluid from pregnant women with previous neural tube defect offspring. Clin. Genet. 1986, 30, 167–172.
-
Magnus, P.; Magnus, E.M.; Berg, K. Transcobalamins in the etiology of neural tube defects. Clin. Genet. 1991, 39, 309–310
-
Low-Beer, etal, 1968 Serum vitamin B12 levels and vitamin B12 binding capacity in pregnant and non-pregnant Europeans and West Indians
PMID 5681054
-
Krishnaveni etal, 2009 Low plasma vitamin B12 in pregnancy is associated with gestational 'diabeity' and later diabetes.
PMID
19707742
-
Lai etal, 2017 High folate and low vitamin B12 status during pregnancy is associated with gestational diabetes
PMID: 28381340
-
Zhang etal, 2016 Decreased levels of vitamin B12 in aging, autism and schizophrenia.
PMID: 26799654
-
Chu etal, 2016 Effects of melatonin and its analogues on neural stem cells. PMID 26499359
-
Rudnitskaya etal, 2015 Melatonin Attenuates Memory Impairment, Amyloid-β Accumulation, and Neurodegeneration in a Rat Model of Sporadic Alzheimer's Disease. PMID 26402759
-
Shen etal, 2016 Effect of Melatonin and Resveratrol against Memory Impairment and Hippocampal Damage in a Rat Model of Vascular Dementia. PMID 28419991
-
Li etal, 2017 Effect of Melatonin on renewal of chick small intestinal mucosa PMID 28431176
-
Rzepka-Migut and Paprocka Efficacy and safety of melatonin treatment in children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity disorder: A review of the literature. Bran Sci 2020 10:219
-
Jin etal Relationship betwee Autism Spectrum Disorder and melatonin during fetal development. Molecules 2018 23:198
-
Whiton etal, 1979 Brain damage in infancy and dietary B12 deficiency PMID 502936
-
Smolka etal, 2001 Metabolic complications and neurological manifestations of vitamin B12 deficiency in children of vegetarian mothers. PMID 11787236
-
Zengin etal, 2008 Clinical manifestations of infants with nutritional vitamin B deficiency due to maternal dietary deficiency PMID 18945280
-
Halicioglu etal, 2011 Nutritional deficiency in infants of vitamin B12 deficient mothers PMID 99429203
-
Demir etal, 2013 Clinical and neurological findings of severe vitamin B12 deficiency... PMID 23781950
-
Kvestad etal Vitamin B12 status in infancy is positively associated with development and cognitive functioning 5 y later in Nepalese children. Am. J. Clin Nut. 2017 105(5):1122-1131
-
Strand etal, The effect of vitamin B12 supplementation in Nepalese infants...Trials, 2017: 187
-
Thomas S, Thomas T, Bosch RJ, Ramthal A, Bellinger DC, Kurpad AV, Duggan CP, Srinivasan K. Effect of Maternal Vitamin B12 Supplementation on Cognitive Outcomes in South Indian Children: A Randomized Controlled Clinical Trial. Matern Child Health J. 2019 Feb;23(2):155-163. doi: 10.1007/s10995-018-2605-z. PMID: 30003521.
-
Chandyo RK, Kvestad I, Ulak M, Ranjitkar S, Hysing M, Shrestha M, Schwinger C, McCann A, Ueland PM, Basnet S, Shrestha L, Strand TA. The effect of vitamin B12 supplementation during pregnancy on infant growth and development in Nepal: a community-based, double-blind, randomised, placebo-controlled trial. Lancet. 2023 May 6;401(10387):1508-1517. doi: 10.1016/S0140-6736(23)00346-X. Epub 2023 Apr 6. PMID: 37031691
-
Strand etal, Maternal and infant vitamin B12 status during infancy predict linear growth at 5 yrs, Ped Res 2018 https://doi.org/10.1038/s41390-018-0072-2
-
Smith, AD 2018 Maternal and infant vitamin B12 status and development. Ped Res. https://doi.org/10.1038/s41390-018-0110-0
-
Guez etal, 2012 Severe vitamin B12 deficiency in an exclusively breastfed 5-month-old Italian infant born to a mother receiving multivitamin supplementation during pregnancy PMC 22726312
-
Roed etal, 2008 Severe vitamin B12 deficiency in infants breastfed by vegans (Ugesr Laeger, 171: 3099-101
-
Shah T, Mishra S, More A, Otiv S, Apte K, Joshi K. Combination of vitamin B12 active forms improved fetal growth in Wistar rats through up-regulation of placental miR-16 and miR-21 levels. Life Sci. 2017 Dec 15;191:97-103. doi: 10.1016/j.lfs.2017.10.017. Epub 2017 Oct 12. PMID: 29032242.
-
Agrawal and Nathani, 2009 Neruo-regression in vitamin B12 deficiency MBJ 2009
-
Saleem TH, Shehata GA, Toghan R, Sakhr HM, Bakri AH, Desoky T, Hamdan FRA, Mohamed NF, Hassan MH. Assessments of Amino Acids, Ammonia and Oxidative Stress Among Cohort of Egyptian Autistic Children: Correlations with Electroencephalogram and Disease Severity. Neuropsychiatr Dis Treat. 2020 Jan 6;16:11-24. doi: 10.2147/NDT.S233105. Erratum in: Neuropsychiatr Dis Treat. 2020 Jan 30;16:325. doi: 10.2147/NDT.S246681. PMID: 32021195; PMCID: PMC6954634.
-
Gutierrez-Diaz, 1959 Effect of magnesium, molybdate, vitamin B12 and vitamin T complex, alone and combined, on development in children. Act Ped Esp. 17; 125-53
-
Schimshaw etal, 1959 Growth and development of Central American children. II The effect of oral administration of vitamin B12 to rural children of preschool and school age. Am J. Clin Nutr. 7: 180-4
-
Chalouhi et al, 2008 Neurological consequences of vitamin B12 deficiency and its treatment. Ped Emerg Care, 24: 538-41
-
Kruithof PD, Lunev S, Aguilar Lozano SP, de Assis Batista F, Al-Dahmani ZM, Joles JA, Dolga AM, Groves MR, van Goor H. Unraveling the role of thiosulfate sulfurtransferase in metabolic diseases. Biochim Biophys Acta Mol Basis Dis. 2020 Jun 1;1866(6):165716. doi: 10.1016/j.bbadis.2020.165716. Epub 2020 Feb 19. PMID: 32061776.
-
Sheng etal, 2019 Effects of dietary intervention on vitamin B12 status and cognitive level of 18 month-old toddlers in high poverty areas...BMC Pert 19:334
-
Smolka etal 2001 Metabolic complications and neurological manifestations of vitamin B12 deficiency in children of vegetarian mothers. Cas Lek Cesk 140: 732-5
-
Lucke et al, 2007 Maternal vitamin B12 deficiency: cause for neurological symptoms in infancy. Z Geburtshilfe Neonatol, 211: 157-161
-
Obeid etal, 2017 Cobalamin status from pregnancy to early childhood.... Adv Nutr 8: 971-979
-
Lovblad etal 1997 Retardation of myelination due to dietary vitamin B12 deficiency: cranial MRI findings Pediatr Radiol 27: 155-8
-
Horstemann etal 2003 Infantile cobalamin deficiency with cerebral lactate accumulation and sustained choline depletion. Neuroped 34; 261-4
-
Rosenblatt etal, 1985 Prenatal vitamin B12 therapy of a fetus with methylcobalamin deficiency. Lancet, 18: 1127-9
-
Graham etal, 1992 Long-term neurologic consequences of nutritional vitamin B12 deficiency in infants. J Ped. 121:710-4
-
Voiculescu etal Role of melatonin in embryo fetal development. 2014. J Med Life 7, 488-492
-
Melke etal. Abnormal melatonin synthesis in autism spectrum disorders. Mol Psychiatry 2008 13, 90-98
-
Goldman etal. Characterizing sleep in adolescents and adults with autism spectrum disorders. J Autism Devel Disorder 2017, 47, 1682-1695
-
Souders etal, Sleep in children with autism spectrum disorders. Curr Psychiatry Rep 2017, 19, 34
-
Geoffray etal. Are circadian rhythms new pathways to understand Autism Spectrum Disorder? J. Physiol Paris 2016, 110, 434-438
-
Cuomo etal Effectiveness of sleep-based interventions for children with Autism Spectrum Disorder. A meta-analysis. Pharmacotherapy 2017, 37, 555-578
-
Huguet etal. The genetics of autism spectrum disorders. 2016, 101-129
-
Braam etal. Low parental melatonin levels increases autism spectrum disorder risk in chidren bioRxiv 2016
-
Stockebrand etal, 2018 A mouse model of creatine transporter deficiency reveals impaired motor function and muscle energy metabolism. Front Physiol 9, 773
-
Braissant etal. Creatine deficiency syndromes and the importance of creatine synthesis in the brain. Amion Acids, 2011 40; 1315-24
-
Perna etal Creatine transporter deficiency leads to increased whole body and cellular metabolism. Amino Aicds 2016 48; 2057-65
-
Udobi eatl, Deletion of the creatine transporter gene in neonatal, but not adult, mice leads to cognitive defects J Inherit Metab Dis. 2019; 42; 966-974
-
Roschel H, Gualano B, Ostojic SM, Rawson ES. Creatine Supplementation and Brain Health. Nutrients. 2021 Feb 10;13(2):586. doi: 10.3390/nu13020586. PMID: 33578876; PMCID: PMC7916590.
-
Renault etal 1999 Neuropathy in two cobalamin-deficient breast-fed infants of vegetarian mothers. Muscle Nerv 22:252-4
-
Nabuurs etal, Disturbed energy metabolism and muscular dystrophy caused by pure creatine deficiency are reversible by creatine intake. J Physiol. 2013 591;571-92
-
Longo etal. Disorders of creatine transport and metabolism. Am J Med Genet C Semin Med Genet 2011 157; 72-8
-
Igbal, F. Review: Human Guanidinoacetate N-methyl Transferase (GAMT) deficiency: A treatable inborn error of metabolism Pak J. Pharm Sci 2015, 28; 2207-11
-
Hall CA 1990 Function of vitamin B12 in the central nervous system as revealed by congenital defects. Am J Hematol. 34:121-7
-
Kosenen and Pihko 1994 Development regression in a child caused by vitamin B12 deficiency. Duodecim. 110: 588-91
-
Monfort-Gouraud et al. 1993 Severe megaloblastic anemia in a child breast fed by a vegetarian mother. Ann Pediatr 40,:28-31
-
von Schenck etal, 1997 Persistence of neurological damage induced by dietary vitamin B12 deficiency in infancy. Arch Dis. Child, 77: 137-9
-
Tashiro etal, 1983 Phosphatidylethanolamine methyltransferase activity in developing, demyelinating, and diabetic mouse brains. Tohuku. J. Exp. Med 141 S485-90
-
Axelrod and Weissbach 1960 Science, 131, 1312
-
Weissbach and Axelrod 1960 J. Fed Proc. 19, 50
-
Weibe etal. Low maternal melatonin level increases Autism Spectrum Disorder Risk in children. Res Deve Disabil 2018 92, 79-89
-
Yunho et al. The relationship between autism spectrum disorder and melatonin during fetal development. Molecules 2018, 23,
-
Gagnon and Godbout Melatonin and comorbidities in children with autism spectrum disorder. Curr Dev Disord Rep 2018, 5, 197-206
-
Mantle etal, 2020 https://www.sciencedirect.com/science/article/pii/S2590142720300112
-
Rossignol and Frye Melatonin in Autism Spectrum Disorders: a systematic review and meta-analysis. Dev Med Child Neurol, 2011, 53, 783-792
-
Rossignol and Frye Melatonin in Autism Spectrum Disorders. Curr Clin Pharmacol 2014 9, 326-34
-
Sanchez-Barcelo et al. Clinical uses of Melatonin in neurological diseases and mental and behavioural disorders Curr Med Chem, 2017 24, 3851-3878
-
Haidar etal. Low oxytocin and melatonin levels and their possible role in the diagnosis and prognosis in Iraqi Autistic children. Saudi Med J. 2016 37, 29-36
-
Blackmer and Feinstein Management of sleep disorders in children with neurodevelopmental disorders: A review Pharmacotherapy. 2016, 36, 84-98
-
Pagan, et al. The serotonin-N-acetylserotonin-melatonin pathway as a biomarker for Autism Spectrum Disorders. Trans Psychiatry, 2014 4, e479
-
Voiculescu et al. Role of melatonin in embryo fetal development. J Med Life. 2014;7(4):488–492
-
Grivas and Savvidou Melatonin the "light of night"...Scoliosis 2007; 2, 6
-
Casella etal, 2005 Vitamin B12 deficiency in infancy as a cause of developmental reqression. Brain Dev. 27: 592-4
-
Aquirre etal, 2019 Serious neurological compromise due to vitamin B12 deficiency in infants of vegan and vegetarian mothers. Arch Argent Pediatr 117
-
Ars etal 2019 Prenatal folate, homocysteine and vitamin B12 levels and child brain volumes. Br J. Nutr. 122: S1-S9.
-
Rose S, Melnyk S, Pavliv O, Bai S, Nick TG, Frye RE, James SJ. Evidence of oxidative damage and inflammation associated with low glutathione redox status in the autism brain. Transl Psychiatry. 2012 Jul 10;2(7):e134. doi: 10.1038/tp.2012.61. PMID: 22781167; PMCID: PMC3410618
-
Black 2008 Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr. Bull. 29: S126-31
-
Renault etal, 1999 Neuropathy in two coblamin-deficient breast-fed infants of vegetarian mothers. Muscle Nerve. 22: 252-4
-
Kanra etal, 2005 Answer to hypotonia: a simple hemogram. J Child Neurol 20: 930-1
-
Stollhoff and Schulte 1987 Vitamin B12 and brain development. Eur J. Pediatr 146: 201-5
-
von Schenck etal 1997 Persistence of neurological damage induced by dietary vitamin B12 deficiency in infancy. Arch Dis Chil 77: 137-9
-
Chandra etal, 2006 Tremors and thrombocytosis during treatment of megaloblastic anaemia. Ann Trop Paediatr 26: 101-5
-
Pawlak etal How prevalent is vitamin B12 deficiency among vegetarians? Nutr Rev. 2013, 72: 220-7
-
Lucke etal, 2007 Maternal vitamin B12 deficiency: cause for neurological symptoms in infancy. Z Gebrurtshilfe Neonatoal 211: 157-61
-
Schlapbach etal, 2007 Floppy baby with macrocytic anemia and vegan mother. Praxis 29: 1309-14
-
Borkowska etal 2007 Vitamin B12 deficiency in a one-year-old, exclusively breast fed child. Med Wieku Rozwoj 11:435-8
-
Chalouhi etal, 2008 Neurological consequences of vitamin B12 deficiency and its treatment. Pediatr Emerg Care 24:538-41
-
Honzik etal, 2010 Clinical presentation and metabolic consequences of 40 breastfed infants with nutritional vitamin B12 deficiency - what have we learned? Eur J Paediatr Neurol 14:488-95
-
Hall 1990 Function of vitamin B12 in the central nevous system as revealed by congenital defects. Am J. Hematol. 34; 121-7
-
Deoni etal. White-matter relaxation time and myelin water fraction differences in young adults with autism. Psychol. Med 2015, 45 795-805
-
Shevell and Rosenblatt 1992 The neurology of cobalamin. Can J Neurol Sci 19: 472-86
-
Strucinska 2002 Vegetarian diets of breastfeeding women in the light of dietary recommendations. Rocz Panstw Zakl Hig 53: 65-79
-
Rendle-Short et al 1979 Vegan mothers with vitamin B12 deficiency. Med J Aust 3:483
-
Michaud et al, 1992 Nutritional vitamin B12 deficiency: two cases detected by routine newborn urinary screening. Eur J Pediatr. 151;218-20
-
Specker 1994 Nutritional concerns of lactating women consuming vegetarian diets. Am J Clin Nutr. 59: 1182S
-
Renault et al 1999 Neuropathy in two cobalamin-deficient breast-fed infants of vegetarian mother. Muscle Nerv 22:252-4
-
Ueland and Monsen 2003 Hyperhomocysteinemia and B-vitamin deficiences in infants and children. Clin Chem Lab Med. 41:1418-26
-
Weiss et al, 2004 Severe vitamin B12 deficiency in an infant associated with maternal deficiency and a strict vegetarian diet. J Ped Hem Oncol. 26:270-1
-
Jarosz et al, 2004 Vitamin B12 deficiency anaemia in a 7.5 months old girl. Med Wieku Rozwoj 8:283-8
-
Baatenburg et al 2006 Developmental delay in breastfed children due to inadequate diet of the mother. Ned Tijdshr Geneeskd 150: 465-9
-
Kollee 2006 Vitamin deficiencies in breastfed children due to maternal dietary deficiency. Ned Tijdschr Geneeskd. 150:473-6
-
Yajnik 2006 Nutritional control of fetal growth. Nutr Rev. 64: S50-1
-
Cetinkaya etal, 2007 Nutritional vitamin B12 deficiency in hospitalized young children. Ped. Hem. Onco. 24:15-21
-
Fadyl and Inoue 2007 Combined B12 and iron deficiency in a child breast-fed by a vegetarian mother. J Ped Hemato Oncol. 29:74
-
Mathey et al, 2007 Failure to thrive and psychomotor regression revealing vitamin B12 deficiency in 3 infants. Arch Ped 14: 467-71
-
Ljungblad UW, Astrup H, Mřrkrid L, Hager HB, Lindberg M, Eklund EA, Bjřrke-Monsen AL, Rootwelt T, Tangeraas T. Breastfed Infants With Spells, Tremor, or Irritability: Rule Out Vitamin B12 Deficiency. Pediatr Neurol. 2022 Jun;131:4-12. doi: 10.1016/j.pediatrneurol.2022.03.003. Epub 2022 Mar 21. PMID: 35439713.
-
Pacheva, I., Ivanov, I., Penkov, M., Kancheva, D., Jordanova, A., & Ivanova, M. (2016). Creatine Deficiency Syndrome could be Missed Easily: A Case Report of Guanidinoacetate Methyltransferase Deficiency Presented with Neurodevelopmental Delay, Seizures, and Behavioral Changes, but Normal Structural MRI. Annals of clinical and laboratory science, 46(5), 557–561.
-
Mercimek-Mahmutoglu S, Stoeckler-Ipsiroglu S, Adami A, Appleton R, Araujo HC, Duran M, et al. GAMT deficiency: features, treatment, and outcome in an inborn error of creatine synthesis. Neurology. 2006;67:480–4.
-
Stockler-Ipsiroglu S, vanKarnebeek CD. Cerebral creatine deficiencies: a group of treatable intellectual developmental disorders. Semin Neurol. 2014;34(3):350-6.
-
Mercimek-Mahmutoglu S, Ndika J, Kanhai W, deVillemeur TB, Cheillan D, Christensen E, et al. Thirteen new patients with guanidinoacetatemethyltransferase deficiency and functional characterization of nineteen novel missense variants in the GAMT gene. HumMutat. 2014;35(4):462-9.
-
O'Rourke DJ, Ryan S, Salomons G, Jakobs C, Monavari A, King MD. Guanidinoacetatemethyltransferase (GAMT) defi[ciency: late onset of movement disorder and preserved expressive language. DevMedChildNeurol. 2009;51:404–7.
-
Caldeira Araújo H, Smit W, Verhoeven NM, Salomons GS, Silva S, Vasconcelos R, Tomás H, TavaresdeAlmeida I, Jakobs C, Duran M. Guanidinoacetate methyltransferase deficiency identified in adults and a child with mental retardation. Am J MedGenet A. 2005;133A:122–
-
Lion-François L, Cheillan D, Pitelet G, Acquaviva-Bourdain C, Bussy G, Cotton F, et al. High frequency of creatine deficiency syndromes in patients with unexplained mental retardation. Neurology. 2006;67:1713–4.
-
Mercimek-Mahmutoglu S, Salomons GS. Creatine Deficiency Syndromes. 2009 Jan 15 [Updated 2015 Dec 10]. In: Pagon RA, Adam MP, Ardinger HH,et al.,editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2016. Available from: http://www.ncbi.nlm.nih.gov/books/NBK3794/
-
Leuzzi V, Mastrangelo M, Battini R, Cioni G.Inborn errors of creatine metabolism and epilepsy. Epilepsia. 2013;54(2):217-27.
-
Schulze A, Hoffmann GF, Bachert P, Kirsch S, Salomons GS, Verhoeven NM, et al. Presymptomatic treatment of neonatal guanidinoacetate methyltransferase deficiency. Neurology. 2006;67:719–21.
-
Verbruggen KT, Sijens PE, Schulze A, Lunsing RJ, Jakobs C, Salomons GS, et al. Successful treatment of a guanidinoacetate methyltransferase deficient patient: findings with relevance to treatment strategy and pathophysiology. MolGenetMetab. 2007b;91:294–6.
-
Morris AA, Appleton RE, Power B, Isherwood DM, Abernethy LJ, Taylor RW, et al. Guanidinoacetate methyltransferase deficiency masquerading as a mitochondrial encephalopathy. J Inherit Metab Dis. 2007; 30(1):100.
-
Item CB, Mercimek-Mahmutoglu S, Battini R, Edlinger-Horvat C, Stromberger C, Bodamer O, et al. Characterization of seven novel mutations in seven patients with GAMT deficiency. Hum Mutat. 2004;23:524.
-
Dror and Allen, 2008 Effect of vitamin B12 deficiency on neurodevelopment in infants... Nutr Rev. 66:250-5
-
Honzik et al, 2010 Clinical presentation and metabolic consequences in 40 breastfed infants... Eur J Paed Neurol. 14:488-95
-
Kocaoglu et al, 2014 Cerebral atrophy in a vitamin B12-deficient infant of a vegetarian mother. J Health Pop Nutr 32:367-71
-
Bousselamati et al. 2018 Psychomotor regression due to vitamin B12 deficiency. Pan Afr MEd J 20:30
-
Bravo etal, 2014 Haematological and neurological compromise due to vitamin B12 deficient in infant of a vegetarian mother.... PMID 25697251
-
Schroder etal 2017 Pregnant women of South Asian Ethnicity in Canada have substantially lower vitamin B12 status compared with pregnant woemen of European ethnicity PMID 28920568
-
Chandyo etal, 2017 The effects of vitamin B12 supplementation during pregnancy PMID 28851784
-
Woods etal, 1960 Vitamin B12Co-60 readily passes the placenta into fetal organs and nursing provides B12 from mother to pup... PMC 2137236
-
Graber etal, 1971 Placental transport of vitamin B12 in the pregnant rat PMID 5552402
-
Michelson etal, 1999 Urinary organic acid screening in children with developmental language delay PMID 10518282
-
Specker et al. 1990 Vitamin B12: Low milk concentrations are related to low serum concentrations in vegetarian women.....Am J Clin Nutr 52:1073-6
-
Specker et al. 1994 Vegetarian diets during lactation. Am J. Clin Nutr 59:1182S-6S
-
Yuge K, Nagamitsu S, Ishikawa Y, Hamada I, Takahashi H, Sugioka H, Yotsuya O, Mishima K, Hayashi M, Yamashita Y. Long-term melatonin treatment for the sleep problems and aberrant behaviors of children with neurodevelopmental disorders. BMC Psychiatry. 2020 Sep 10;20(1):445. doi: 10.1186/s12888-020-02847-y. PMID: 32912180; PMCID: PMC7488027.
-
Ming X, Walters AS. Autism spectrum disorders, attention deficit/hyperactivity disorder, and sleep disorders. Curr Opin Pulm Med. 2009 Nov;15(6):578-84. doi: 10.1097/MCP.0b013e3283319a9a. PMID: 19713848.
-
Malow BA. Sleep disorders, epilepsy, and autism. Ment Retard Dev Disabil Res Rev. 2004;10(2):122-5. doi: 10.1002/mrdd.20023. PMID: 15362168.
-
Goraya etal. Neuroloty of nutrition vitamin B12 deficiency also known as "infantile tremor syndrome". J Clin Neurol. 2015 30, 1831-7
-
Daphna etl Effect of vitamin B12 deficiency on neurodevelopment in infants: current knowledge and possible mechanisms. Nutr Rev. 2008 55:250-5
-
Chalouhi etal. Neurological consequences of vitamin B12 deficiency and its treatment. Pediatr Emerg Care. 2008 24P538-41
-
Davis and Melina 2014 Becoming vegan: comprehensive addition.
-
Strand etal, 2015 Vitamin B12, folic acid, and growth in 6- to 30-month-old children... Pediatrics 135;918-26
-
Lázár AS, Bódizs R. Az alvás szerkezete és mintázatai autizmus spektrumzavarban [The structure and patterns of sleep in autism spectrum disorders]. Psychiatr Hung. 2008;23(2):109-28. Hungarian. PMID: 18956612.
-
Peneles etal, 2010 Vitamin B12 optic neuropathy in autism Pediatrics 125 e967-3970.
-
Chang etal, 2020 Prevalence of opthalmologic diagnoses in children with autism spectrum disorder... Am J Opthalmol. 4; S0002
-
Benbir etal, 2007 Seizures during treatment of vitamin B12 deficiency. Seizure. 2007 Jan;16(1):69-73. Epub 2006 Dec 5
-
Abdulamir etal. Low oxytocin and melatonin levels and their possible role in the diagnosis and prognosis in Iraqi autistic children. Saudi Med J. 2016 37, 29-36
-
Fry et al Treatment of folate abnormalities in Autism Spectrum Disorder. Seminars in Paediatric Neurology. 2020 in press.
-
Conrad AL, Wermke K, Eisenmann M, Kuhlmann E, Benavides A, Koscik T, Magnotta V. Preliminary evaluation of pre-speech and neurodevelopmental measures in 7-11-week-old infants with isolated oral clefts. Pediatr Res. 2021 Jan;89(1):85-90. doi: 10.1038/s41390-020-0887-5. Epub 2020 Apr 12. PMID: 32279071; PMCID: PMC7554202.
-
Wang J, Yang Y, Zhao X, Zuo Z, Tan LH. Evolutional and developmental anatomical architecture of the left inferior frontal gyrus. Neuroimage. 2020 Nov 15;222:117268. doi: 10.1016/j.neuroimage.2020.117268. Epub 2020 Aug 18. PMID: 32818615.
-
Brauer J, Anwander A, Friederici AD. Neuroanatomical prerequisites for language functions in the maturing brain. Cereb Cortex. 2011 Feb;21(2):459-66. doi: 10.1093/cercor/bhq108. Epub 2010 Jun 21. PMID: 20566580.
-
Su P, Kuan CC, Kaga K, Sano M, Mima K. Myelination progression in language-correlated regions in brain of normal children determined by quantitative MRI assessment. Int J Pediatr Otorhinolaryngol. 2008 Dec;72(12):1751-63. doi: 10.1016/j.ijporl.2008.05.017. Epub 2008 Oct 11. PMID: 18849083.
-
Hahn A, Kranz GS, Sladky R, Kaufmann U, Ganger S, Hummer A, Seiger R, Spies M, Vanicek T, Winkler D, Kasper S, Windischberger C, Swaab DF, Lanzenberger R. Testosterone affects language areas of the adult human brain. Hum Brain Mapp. 2016 May;37(5):1738-48. doi: 10.1002/hbm.23133. Epub 2016 Feb 15. PMID: 26876303; PMCID: PMC4949561.
-
Moore S, Meschkat M, Ruhwedel T, Trevisiol A, Tzvetanova ID, Battefeld A, Kusch K, Kole MHP, Strenzke N, Möbius W, de Hoz L, Nave KA. A role of oligodendrocytes in information processing. Nat Commun. 2020 Oct 30;11(1):5497. doi: 10.1038/s41467-020-19152-7. PMID: 33127910; PMCID: PMC7599337.
-
Flöel A, de Vries MH, Scholz J, Breitenstein C, Johansen-Berg H. White matter integrity in the vicinity of Broca's area predicts grammar learning success. Neuroimage. 2009 Oct 1;47(4):1974-81. doi: 10.1016/j.neuroimage.2009.05.046. Epub 2009 May 27. PMID: 19477281.
-
McDonagh MS, Holmes R, Hsu F. Pharmacologic Treatments for Sleep Disorders in Children: A Systematic Review. J Child Neurol. 2019 Apr;34(5):237-247. doi: 10.1177/0883073818821030. Epub 2019 Jan 23. PMID: 30674203.
-
Accardo JA, Malow BA. Sleep, epilepsy, and autism. Epilepsy Behav. 2015 Jun;47:202-6. doi: 10.1016/j.yebeh.2014.09.081. Epub 2014 Dec 10. PMID: 25496798.
-
Johnson KP, Zarrinnegar P. Autism Spectrum Disorder and Sleep. Child Adolesc Psychiatr Clin N Am. 2021 Jan;30(1):195-208. doi: 10.1016/j.chc.2020.08.012. PMID: 33223062.
-
Pévet P, Balemans MG, Legerstee WC, Vivien-Roels B. Circadian rhythmicity of the activity of hydroxyindole-O-methyl transferase (HIOMT) in the formation of melatonin and 5-methoxytryptophol in the pineal, retina, and harderian gland of the golden hamster. J Neural Transm. 1980;49(4):229-45. doi: 10.1007/BF01252128. PMID: 7463036.
-
James etal Abnormal transmethylation/transulfation metabolism and DNA hypomethylation among parents of children with autism. J. Autism Dev Discord 2008: 39:1966-75.
-
Indika NR, Deutz NEP, Engelen MPKJ, Peiris H, Wijetunge S, Perera R. Sulfur amino acid metabolism and related metabotypes of autism spectrum disorder: A review of biochemical evidence for a hypothesis. Biochimie. 2021 May;184:143-157. doi: 10.1016/j.biochi.2021.02.018. Epub 2021 Mar 4. PMID: 33675854.
-
Guo BQ, Ding SB, Li HB. Blood biomarker levels of methylation capacity in autism spectrum disorder: a systematic review and meta-analysis. Acta Psychiatr Scand. 2020 Jun;141(6):492-509. doi: 10.1111/acps.13170. Epub 2020 Apr 6. PMID: 32173856.
-
James SJ, Cutler P, Melnyk S, Jernigan S, Janak L, Gaylor DW, Neubrander JA. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004 Dec;80(6):1611-7. doi: 10.1093/ajcn/80.6.1611. PMID: 15585776.
-
Lu SC. Regulation of glutathione synthesis. Mol Aspects Med 2009;30:42-59.
-
Frye, wr al (2018). Folinic acid improves verbal communication in children with autism and language impairment: a randomized double-blind placebo-controlled trial. Molecular psychiatry, 23(2), 247–256. https://doi.org/10.1038/mp.2016.168
-
Mezzacappa, A., Lasica, P. A., Gianfagna, F., Cazas, O., Hardy, P., Falissard, B., Sutter-Dallay, A. L., & Gressier, F. (2017). Risk for Autism Spectrum Disorders According to Period of Prenatal Antidepressant Exposure: A Systematic Review and Meta-analysis. JAMA pediatrics, 171(6), 555–563. https://doi.org/10.1001/jamapediatrics.2017.0124
-
Pedersen L. H. (2015). Prenatal Antidepressant Exposure and Childhood Autism Spectrum Disorders: Cause for Concern?. Paediatric drugs, 17(6), 443–448. https://doi.org/10.1007/s40272-015-0141-5
-
Sujan, A. C., Rickert, M. E., Öberg, A. S., Quinn, P. D., Hernández-Díaz, S., Almqvist, C., Lichtenstein, P., Larsson, H., & D'Onofrio, B. M. (2017). Associations of Maternal Antidepressant Use During the First Trimester of Pregnancy With Preterm Birth, Small for Gestational Age, Autism Spectrum Disorder, and Attention-Deficit/Hyperactivity Disorder in Offspring. JAMA, 317(15), 1553–1562. https://doi.org/10.1001/jama.2017.3413
-
Brown, H. K., Ray, J. G., Wilton, A. S., Lunsky, Y., Gomes, T., & Vigod, S. N. (2017). Association Between Serotonergic Antidepressant Use During Pregnancy and Autism Spectrum Disorder in Children. JAMA, 317(15), 1544–1552. https://doi.org/10.1001/jama.2017.3415
-
Becker M, Weinberger T, Chandy A, Schmukler S. (2016) Depression During Pregnancy and Postpartum. Curr Psychiatry Rep. Mar;18(3):32. doi: 10.1007/s11920-016-0664-7. PMID: 26879925.
-
Morales DR, Slattery J, Evans S, Kurz X. Antidepressant use during pregnancy and risk of autism spectrum disorder and attention deficit hyperactivity disorder: systematic review of observational studies and methodological
considerations. BMC Med. 2018 Jan 15;16(1):6. doi: 10.1186/s12916-017-0993-3. PMID: 29332605; PMCID: PMC5767968. -
Sujan AC, Rickert ME, Öberg AS, Quinn PD, Hernández-Díaz S, Almqvist C, Lichtenstein P, Larsson H, D'Onofrio BM. Associations of Maternal Antidepressant Use During the First Trimester of Pregnancy With Preterm Birth, Small for
Gestational Age, Autism Spectrum Disorder, and Attention-Deficit/Hyperactivity Disorder in Offspring. JAMA. 2017 Apr 18;317(15):1553-1562. doi: 10.1001/jama.2017.3413. PMID: 28418479; PMCID: PMC5875187. -
Andrade C. Antidepressant Exposure During Pregnancy and Risk of Autism in the Offspring, 1: Meta-Review of Meta-Analyses. J Clin Psychiatry. 2017 Sep/Oct;78(8):e1047-e1051. doi: 10.4088/JCP.17f11903. PMID: 28994903.
-
Rai D, Lee BK, Dalman C, Newschaffer C, Lewis G, Magnusson C. Antidepressants during pregnancy and autism in offspring: population based cohort study. BMJ. 2017 Jul 19;358:j2811. doi: 10.1136/bmj.j2811. PMID: 28724519; PMCID:
PMC5516223. -
Rai D, Lee BK, Dalman C, Golding J, Lewis G, Magnusson C. Parental depression, maternal antidepressant use during pregnancy, and risk of autismspectrum disorders: population based case-control study. BMJ. 2013 Apr 19;346:f2059. doi: 10.1136/bmj.f2059. PMID: 23604083; PMCID: PMC3630989.
-
Viktorin A, Uher R, Kolevzon A, Reichenberg A, Levine SZ, Sandin S. Association of Antidepressant Medication Use During Pregnancy With Intellectual Disability in Offspring. JAMA Psychiatry. 2017 Oct 1;74(10):1031-1038. doi: 10.1001/jamapsychiatry.2017.1727. PMID: 28700807; PMCID: PMC5710466.
-
Yamamoto-Sasaki M, Yoshida S, Takeuchi M, Tanaka-Mizuno S, Ogawa Y, Furukawa TA, Kawakami K. Association between antidepressant use during pregnancy and autism spectrum disorder in children: a retrospective cohort study based on
Japanese claims data. Matern Health Neonatol Perinatol. 2019 Jan 10;5:1. doi: 10.1186/s40748-018-0096-y. PMID: 30652008; PMCID: PMC6327597. -
Hagberg KW, Robijn AL, Jick S. Maternal depression and antidepressant use during pregnancy and the risk of autism spectrum disorder in offspring. Clin Epidemiol. 2018 Nov 1;10:1599-1612. doi: 10.2147/CLEP.S180618. PMID: 30464639;
PMCID: PMC6219268. -
Andrade C. Antidepressant Exposure During Pregnancy and Risk of Autism in the Offspring, 2: Do the New Studies Add Anything New? J Clin Psychiatry. 2017 Sep/Oct;78(8):e1052-e1056. doi: 10.4088/JCP.17f11916. PMID: 29099558.
-
Zhou XH, Li YJ, Ou JJ, Li YM. Association between maternal antidepressant use during pregnancy and autism spectrum disorder: an updated meta-analysis. Mol Autism. 2018 Mar 27;9:21. doi: 10.1186/s13229-018-0207-7. PMID: 29599960; PMCID: PMC5870683.
-
Youness, E. R., Shady, M., Abd Elaziz, A., Galal, E., El-Sonbaty, M., El-Sonbaty, M. M., Masoud, M. M., & Abu Elhamd, W. A. (2020). Association of folic acid, vitamin B12, and intelligence scores in epileptic children. Applied neuropsychology. Child, 1–5. Advance online publication. https://doi.org/10.1080/21622965.2020.1747020
-
Li, X. H., Hou, X. Y., & Chen, R. (2015). The roles of vitamin B12 and vitamin D in children with intractable epilepsy. International journal of clinical and experimental medicine, 8(1), 764–769.
-
Dinç, D., & Schulte, P. (2018). Invloed van anti-epileptica op foliumzuur-, vitamine B12- en homocysteďnewaarden [The use of anticonvulsants and the levels of folate, vitamin B12 and homocysteine]. Tijdschrift voor psychiatrie, 60(1), 20–28.
-
Silva, B., Velosa, A., & Barahona-Corręa, J. B. (2019). Reversible dementia, psychotic symptoms and epilepsy in a patient with vitamin B12 deficiency. BMJ case reports, 12(5), e229044. https://doi.org/10.1136/bcr-2018-229044
-
Glaser, K., Girschick, H. J., Schropp, C., & Speer, C. P. (2015). Psychomotor development following early treatment of severe infantile vitamin B12 deficiency and West syndrome--is everything fine? A case report and review of literature. Brain & development, 37(3), 347–351. https://doi.org/10.1016/j.braindev.2014.05.006
-
Matsumoto, A., Shiga, Y., Shimizu, H., Kimura, I., & Hisanaga, K. (2009). Rinsho shinkeigaku = Clinical neurology, 49(4), 179–185. https://doi.org/10.5692/clinicalneurol.49.179
-
Diaz-Arrastia R. (2000). Homocysteine and neurologic disease. Archives of neurology, 57(10), 1422–1427. https://doi.org/10.1001/archneur.57.10.1422
-
Meena, M. K., Sharma, S., Bhasin, H., Jain, P., Kapoor, S., Jain, A., & Aneja, S. (2018). Vitamin B12 Deficiency in Children With Infantile Spasms: A Case-Control Study. Journal of child neurology, 33(12), 767–771. https://doi.org/10.1177/0883073818787062
-
Ma, X., Zhang, Y., Yang, Y., Liu, X., Yang, Z., Bao, X., Qin, J., & Wu, X. (2011). Epilepsy in children with methylmalonic acidemia: electroclinical features and prognosis. Brain & development, 33(9), 790–795. https://doi.org/10.1016/j.braindev.2011.06.001
-
Aslan, K., Bozdemir, H., Unsal, C., & Güvenc, B. (2008). The effect of antiepileptic drugs on vitamin B12 metabolism. International journal of laboratory hematology, 30(1), 26–35. https://doi.org/10.1111/j.1751-553X.2007.00910.x
-
Korenke, G. C., Hunneman, D. H., Eber, S., & Hanefeld, F. (2004). Severe encephalopathy with epilepsy in an infant caused by subclinical maternal pernicious anaemia: case report and review of the literature. European journal of pediatrics, 163(4-5), 196–201. https://doi.org/10.1007/s00431-004-1402-4
-
Zaric BL, Obradovic M, Bajic V, etal Homocysteine and Hyperhomocysteinaemia. Curr Med Chem. 2019; 26, 2948-2961.
-
Souders MC, Zavodny S, Eriksen W, Sinko R, Connell J, Kerns C, Schaaf R, Pinto-Martin J. Sleep in Children with Autism Spectrum Disorder. Curr Psychiatry Rep. 2017 Jun;19(6):34. doi: 10.1007/s11920-017-0782-x. PMID: 28502070; PMCID: PMC5846201.
-
Moore, E, Mander A, Ames D, Carner, R. etal Cognitive impairment and vitamin B12: a review. Int Psychogeriatr. 2012; 24, 541-556 soi:10.1017/S1041610211002511
-
Naerland, T., Hřiland, A. L., Torske, T., Malt, E., Abrahamsen, T., Nerhus, M., Wedervang-Resell, K., Lonning, V., Johannessen, J., Steen, N. E., Agartz, I., Stenberg, N., Hundhausen, T., Mřrkrid, L., & Andreassen, O. A. (2020). Higher vitamin B12 levels in neurodevelopmental disorders than in healthy controls and schizophrenia: A comparison among participants between 2 and 53 years. FASEB journal : official publication of the Federation of American Societies for Experimental Biology, 34(6), 8114–8124. https://doi.org/10.1096/fj.201900855RRR
Chalouhi C, Faesch S, Anthoine-Milhomme MC, Fulla Y, Dulac O, Chéron G. Neurological consequences of vitamin B12 deficiency and its treatment. Pediatr Emerg Care. 2008 Aug;24(8):538-41. doi: 10.1097/PEC.0b013e318180ff32. PMID: 18708898.
Demir N, Koc A, Üstyol L, Peker E, Abuhandan M. Clinical and neurological findings of severe vitamin B12 deficiency in infancy and importance of early diagnosis and treatment. J Paediatr Child Health. 2013 Oct;49(10):820-4. doi: 10.1111/jpc.12292. Epub 2013 Jun 18. PMID: 23781950.
Bousselamti A, El Hasbaoui B, Echahdi H, Krouile Y. Psychomotor regression due to vitamin B12 deficiency. Pan Afr Med J. 2018 Jun 20;30:152. doi: 10.11604/pamj.2018.30.152.12046. PMID: 30374398; PMCID: PMC6201603.
Acıpayam C, Güneş H, Güngör O, İpek S, Sarışık N, Demir NŞ. Cerebral atrophy in 21 hypotonic infants with severe vitamin B12 deficiency. J Paediatr Child Health. 2020 May;56(5):751-756. doi: 10.1111/jpc.14733. Epub 2019 Dec 23. PMID: 31868292.
Akcaboy M, Malbora B, Zorlu P, Altınel E, Oguz MM, Senel S. Vitamin B12 Deficiency in Infants. Indian J Pediatr. 2015 Jul;82(7):619-24. doi: 10.1007/s12098-015-1725-3. Epub 2015 Apr 5. PMID: 25840526
Serin HM, Arslan EA. Neurological symptoms of vitamin B12 deficiency: analysis of pediatric patients. Acta Clin Croat. 2019 Jun;58(2):295-302. doi: 10.20471/acc.2019.58.02.13. PMID: 31819326; PMCID: PMC6884369.
Incecik F, Hergüner MO, Altunbaşak S, Leblebisatan G. Neurologic findings of nutritional vitamin B12 deficiency in children. Turk J Pediatr. 2010 Jan-Feb;52(1):17-21. PMID: 20402062.
Honzik T, Adamovicova M, Smolka V, Magner M, Hruba E, Zeman J. Clinical presentation and metabolic consequences in 40 breastfed infants with nutritional vitamin B12 deficiency--what have we learned? Eur J Paediatr Neurol. 2010 Nov;14(6):488-95. doi: 10.1016/j.ejpn.2009.12.003. Epub 2010 Jan 20. PMID: 20089427.
Bicakci Z. Growth retardation, general hypotonia, and loss of acquired neuromotor skills in the infants of mothers with cobalamin deficiency and the possible role of succinyl-CoA and glycine in the pathogenesis. Medicine (Baltimore). 2015 Mar;94(9):e584. doi:
Smolka V, Bekárek V, Hlídková E, Bucil J, Mayerová D, Skopková Z, Adam T, Hrubá E, Kozich V, Buriánková L, Saligová J, Buncová M, Zeman J. Metabolické komplikace a neurologické projevy pri deficitu vitaminu B12 u dĕtí vegetariánských matek [Metabolic complications and neurologic manifestations of vitamin B12 deficiency in children of vegetarian mothers]. Cas Lek Cesk. 2001 Nov 22;140(23):732-5. Czech. PMID: 11787236.
Taskesen M, Yaramis A, Pirinccioglu AG, Ekici F. Cranial magnetic resonance imaging findings of nutritional vitamin B12 deficiency in 15 hypotonic infants. Eur J Paediatr Neurol. 2012 May;16(3):266-70. doi: 10.1016/j.ejpn.2011.08.005. Epub 2011 Sep 7. PMID: 21903432.
Gupta R, Rawat AK, Singh P, Gupta J, Pathak A. Infantile tremor syndrome: current perspectives. Res Rep Trop Med. 2019 Jul 5;10:103-108. doi: 10.2147/RRTM.S180604. PMID: 31308787; PMCID: PMC6615725.
Benbir G, Uysal S, Saltik S, Zeybek CA, Aydin A, Dervent A, Yalcinkaya C. Seizures during treatment of Vitamin B12 deficiency. Seizure. 2007 Jan;16(1):69-73. doi: 10.1016/j.seizure.2006.10.016. Epub 2006 Dec 5. PMID: 17150378.
Vieira D, Florindo C, Tavares de Almeida I, Macário MC. Adult-onset methylenetetrahydrofolate reductase deficiency. BMJ Case Rep. 2020 Mar 10;13(3):e232241. doi: 10.1136/bcr-2019-232241. PMID: 32161077; PMCID: PMC7066602.
Bădescu GM, Fîlfan M, Sandu RE, Surugiu R, Ciobanu O, Popa-Wagner A. Molecular mechanisms underlying neurodevelopmental disorders, ADHD and autism. Rom J Morphol Embryol. 2016;57(2):361-6. PMID: 27516006.
Oslejskova H, Dusek L, Makovska Z, Rektor I. Epilepsia, epileptiform abnormalities, non-right-handedness, hypotonia and severe decreased IQ are associated with language impairment in autism. Epileptic Disord. 2007 Dec;9 Suppl 1:S9-18. doi: 10.1684/epd.2007.0154. PMID: 18319196.
Lopez-Espejo MA, Nuńez AC, Moscoso OC, Escobar RG. Clinical characteristics of children affected by autism spectrum disorder with and without generalized hypotonia. Eur J Pediatr. 2021 Oct;180(10):3243-3246. doi: 10.1007/s00431-021-04038-7. Epub 2021 Apr 14. PMID: 33855616.
Gabis LV, Shaham M, Leon Attia O, Shefer S, Rosenan R, Gabis T, Daloya M. The Weak Link: Hypotonia in Infancy and Autism Early Identification. Front Neurol. 2021 Feb 4;12:612674. doi: 10.3389/fneur.2021.612674. PMID: 33613430; PMCID: PMC7891038.
GAMT deficiency References
-
Guanidinoacetate methyltransferase deficiency. Genetics Home Reference. June 2015; http://ghr.nlm.nih.gov/condition/guanidinoacetate-methyltransferase-deficiency.
-
Mercimek-Mahmutoglu S, Salomons GS. Creatine Deficiency Syndromes. GeneReviews. Updated Dec. 10, 2015; https://www.ncbi.nlm.nih.gov/books/NBK3794.
-
Stockler-Ipsiroglu S, vet al Guanidinoacetate methyltransferase (GAMT) deficiency: outcomes in 48 individuals and recommendations for diagnosis, treatment, and monitoring. Molecular Genetics and Metabolism.. January 2014; 111(1):16-25. https://www.ncbi.nlm.nih.gov/pubmed/24268530.
-
Cerebral Creatine Deficiency Syndrome2; CCDS2. Online Mendelian Inheritance in Man. June 18, 2014; https://www.omim.org/entry/612736.
-
Iqbal F. Review: Human guanidinoacetate n-methyl transferase (GAMT) deficiency: A treatable inborn error of metabolism. Pakistan Journal of Pharmaceutical Sciences. November 2015; 28(6):2207-2211. https://www.ncbi.nlm.nih.gov/pubmed/26639513.
-
Stockler S. Guanidinoacetate methyltransferase deficiency. Orphanet. December 2014; http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=382
-
Singer, HS.etal Inherited Metabolic Disorders with Associated Movement Abnormalities in Movement Disorders in Childhood (Second Edition), 2016
-
Sun, Q. Cerebral creatine deficiency syndromes in Biomarkers in Inborn Errors of Metabolism, 2017
Nitrous Oxide and Vitamin B12 deficiency
Neveu J, Perelman S, Suisse G, Monpoux F. Severe hyperhomocysteinemia and peripheral neuropathy as side effects of nitrous oxide in two patients with
sickle cell disease. Arch Pediatr. 2019 Oct;26(7):419-421. doi: 10.1016/j.arcped.2019.09.006. Epub 2019 Oct 17. PubMed PMID: 31630905.
Edigin E, Ajiboye O, Nathani A. Nitrous Oxide-induced B12 Deficiency Presenting With Myeloneuropathy. Cureus. 2019 Aug 6;11(8):e5331. doi:10.7759/cureus.5331. PubMed PMID: 31598438; PubMed Central PMCID: PMC6777927.
Tani J, Weng HY, Chen HJ, Chang TS, Sung JY, Lin CS. Elucidating Unique Axonal Dysfunction Between Nitrous Oxide Abuse and Vitamin B12 Deficiency. Front Neurol. 2019 Jul 9;10:704. doi: 10.3389/fneur.2019.00704. eCollection 2019. PubMed PMID: 31354607; PubMed Central PMCID: PMC6633399.
Nouri A, Patel K, Montejo J, Nasser R, Gimbel DA, Sciubba DM, Cheng JS. The Role of Vitamin B(12) in the Management and Optimization of Treatment in Patients With Degenerative Cervical Myelopathy. Global Spine J. 2019 May;9(3):331-337. doi: 10.1177/2192568218758633. Epub 2018 May 17. Review. PubMed PMID: 31192102; PubMed Central PMCID: PMC6542160.
Gullestrup A, Jensen RB, Břgevig S, Nilsson PM. [Acute neuropathy and liver injury following the abuse of nitrous oxide]. Ugeskr Laeger. 2019 May 13;181(20).
pii: V12180890. Danish. PubMed PMID: 31124452.
Norris F, Mallia P. Lesson of the month 2: A case of nitrous oxide-induced pancytopenia. Clin Med (Lond). 2019 Mar;19(2):129-130. doi: 10.7861/clinmedicine.19-2-129. PubMed PMID: 30872294; PubMed Central PMCID:
PMC6454366.
Williamson J, Huda S, Damodaran D. Nitrous oxide myelopathy with functional vitamin B (12) deficiency. BMJ Case Rep. 2019 Feb 13;12(2). pii: e227439. doi:
10.1136/bcr-2018-227439. PubMed PMID: 30765444.
Lundin MS, Cherian J, Andrew MN, Tikaria R. One month of nitrous oxide abuse causing acute vitamin B (12) deficiency with severe neuropsychiatric symptoms.
BMJ Case Rep. 2019 Feb 7;12(2). pii: bcr-2018-228001. doi: 10.1136/bcr-2018-228001. PubMed PMID: 30737329.
Lan SY, Kuo CY, Chou CC, Kong SS, Hung PC, Tsai HY, Chen YC, Lin JJ, Chou IJ, Lin KL; PCHAN Study Group. Recreational nitrous oxide abuse related subacute combined degeneration of the spinal cord in adolescents - A case series and literature review. Brain Dev. 2019 May;41(5):428-435. doi: 10.1016/j.braindev.2018.12.003. Epub 2019 Jan 2. Review. PubMed PMID: 30611595.
Dong X, Ba F, Wang R, Zheng D. Imaging appearance of myelopathy secondary to nitrous oxide abuse: a case report and review of the literature. Int J Neurosci.
2019 Mar;129(3):225-229. doi: 10.1080/00207454.2018.1526801. Epub 2018 Dec 4.Review. PubMed PMID: 30234413.
Patel KK, Mejia Munne JC, Gunness VRN, Hersey D, Alshafai N, Sciubba D, Nasser R, Gimbel D, Cheng J, Nouri A. Subacute combined degeneration of the
spinal cord following nitrous oxide anesthesia: A systematic review of cases. Clin Neurol Neurosurg. 2018 Oct;173:163-168. doi: 10.1016/j.clineuro.2018.08.016.
Epub 2018 Aug 9. Erratum in: Clin Neurol Neurosurg. 2019 Feb;177:123-124. Abstract corrected. PubMed PMID: 30144777.
Jolobe OMP. Other aspects of nitrous oxide-related neuromyelopathy. Am J Emerg Med. 2019 Feb;37(2):350-351. doi: 10.1016/j.ajem.2018.05.076. Epub 2018 May 30. PubMed PMID: 29866413.
Egan W, Steinberg E, Rose J. Vitamin B(12) deficiency-induced neuropathy secondary to prolonged recreational use of nitrous oxide. Am J Emerg Med. 2018
Sep;36(9):1717.e1-1717.e2. doi: 10.1016/j.ajem.2018.05.029. Epub 2018 May 24. PubMed PMID: 29859645.
Anderson D, Beecher G, van Dijk R, Hussain M, Siddiqi Z, Ba F. Subacute Combined Degeneration from Nitrous Oxide Abuse in a Patient with Pernicious
Anemia. Can J Neurol Sci. 2018 May;45(3):334-335. doi: 10.1017/cjn.2018.15. PubMed PMID: 29756593.
Antonucci MU. Subacute Combined Degeneration from Recreational Nitrous Oxide Inhalation. J Emerg Med. 2018 May;54(5):e105-e107. doi: 10.1016/j.jemermed.2018.01.045. Epub 2018 Mar 27. PubMed PMID: 29602528.
Keddie S, Adams A, Kelso ARC, Turner B, Schmierer K, Gnanapavan S, Malaspina A, Giovannoni G, Basnett I, Noyce AJ. No laughing matter: subacute degeneration of the spinal cord due to nitrous oxide inhalation. J Neurol. 2018 May;265(5):1089-1095. doi: 10.1007/s00415-018-8801-3. Epub 2018 Mar 3. PubMed
PMID: 29502317; PubMed Central PMCID: PMC5937900.
Johnson K, Mikhail P, Kim MG, Bosco A, Huynh W. Recreational nitrous oxide-associated neurotoxicity. J Neurol Neurosurg Psychiatry. 2018 Aug;89(8):897-898. doi: 10.1136/jnnp-2017-317768. Epub 2018 Jan 24. PubMed PMID: 29367261.
Al-Sadawi M, Claris H, Archie C, Jayarangaiah A, Oluya M, McFarlane SI. Inhaled Nitrous Oxide 'Whip-Its!' Causing Subacute Combined Degeneration of
Spinal Cord. Am J Med Case Rep. 2018;6(12):237-240. doi: 10.12691/ajmcr-6-12-3. Epub 2018 Dec 26. PubMed PMID: 31058215; PubMed Central PMCID: PMC6499494.
Friedlander G, Davies T. The Last Laugh - Reversible myeloneuropathy induced by chronic nitrous oxide use. Acute Med. 2018;17(4):232-235. PubMed PMID:
30882108.
Yuan JL, Wang SK, Jiang T, Hu WL. Nitrous oxide induced subacute combined degeneration with longitudinally extensive myelopathy with inverted V-sign on
spinal MRI: a case report and literature review. BMC Neurol. 2017 Dec 28;17(1):222. doi: 10.1186/s12883-017-0990-3. PubMed PMID: 29282001; PubMed
Central PMCID: PMC5745895.
Conjaerts SHP, Bruijnes JE, Beerhorst K, Beekman R. [Nitrous oxide-induced polyneuropathy]. Ned Tijdschr Geneeskd. 2017;161:D2044. Dutch. PubMed PMID:
29192578.
Kaski D, Kumar P, Murphy E, Warner TT. Iatrogenic B12-deficient peripheral neuropathy following nitrous oxide administration for functional tonic leg spasm:
A case report. Clin Neurol Neurosurg. 2017 Sep;160:108-110. doi:10.1016/j.clineuro.2017.07.006. Epub 2017 Jul 6. PubMed PMID: 28709008.
Stockton L, Simonsen C, Seago S. Nitrous oxide-induced vitamin B12 deficiency. Proc (Bayl Univ Med Cent). 2017 Apr;30(2):171-172. PubMed PMID: 28405070; PubMed Central PMCID: PMC5349816.
Buizert A, Sharma R, Koppen H. When the Laughing Stops: Subacute Combined Spinal Cord Degeneration Caused by Laughing Gas Use. J Addict Med. 2017
May/Jun;11(3):235-236. doi: 10.1097/ADM.0000000000000295. PubMed PMID: 28166085.
40: Chen HJ, Huang CS. Nitrous Oxide-induced Subacute Combined Degeneration Presenting with Dystonia and Pseudoathetosis: A Case Report. Acta Neurol Taiwan. 2016 Jun 15;25(2):50-55. PubMed PMID: 27854092.
Mancke F, Kaklauskaitė G, Kollmer J, Weiler M. Psychiatric comorbidities in a young man with subacute myelopathy induced by abusive nitrous oxide consumption: a case report. Subst Abuse Rehabil. 2016 Sep 29;7:155-159. eCollection 2016.PubMed PMID: 27729826; PubMed Central PMCID: PMC5047713.
Massey TH, Pickersgill TT, J Peall K. Nitrous oxide misuse and vitamin B12 deficiency. BMJ Case Rep. 2016 May 31;2016. pii: bcr2016215728. doi:10.1136/bcr-2016-215728. PubMed PMID: 27247211; PubMed Central PMCID: PMC4904416.
Duque MA, Kresak JL, Falchook A, Harris NS. Nitrous Oxide Abuse and Vitamin B12 Action in a 20-Year-Old Woman: A Case Report. Lab Med. 2015 Fall;46(4):312-5. doi: 10.1309/LM0L9HAVXCHF1UQM. PubMed PMID: 26489675.
Pugliese RS, Slagle EJ, Oettinger GR, Neuburger KJ, Ambrose TM. Subacute combined degeneration of the spinal cord in a patient abusing nitrous oxide and
self-medicating with cyanocobalamin. Am J Health Syst Pharm. 2015 Jun 1;72(11):952-7. doi: 10.2146/ajhp140583. PubMed PMID: 25987690.
Morris N, Lynch K, Greenberg SA. Severe motor neuropathy or neuronopathy due to nitrous oxide toxicity after correction of vitamin B12 deficiency. Muscle
Nerve. 2015 Apr;51(4):614-6. doi: 10.1002/mus.24482. Epub 2015 Feb 24. PubMedPMID: 25297001.
Garakani A, Welch AK, Jaffe RJ, Protin CA, McDowell DM. Psychosis and low cyanocobalamin in a patient abusing nitrous oxide and cannabis. Psychosomatics.
2014 Nov-Dec;55(6):715-9. doi: 10.1016/j.psym.2013.11.001. Epub 2013 Nov 5.PubMed PMID: 24367897.
Safari A, Emadi F, Jamali E, Borhani-Haghighi A. Clinical and MRI manifestations of nitrous oxide induced vitamin B12 deficiency: A case report. Iran J Neurol. 2013;12(3):111-3. PubMed PMID: 24250916; PubMed Central PMCID: PMC3829298.
Chiang TT, Hung CT, Wang WM, Lee JT, Yang FC. Recreational nitrous oxide abuse-induced vitamin B12 deficiency in a patient presenting with
hyperpigmentation of the skin. Case Rep Dermatol. 2013 Jun 29;5(2):186-91. doi: 10.1159/000353623. Print 2013 May. PubMed PMID: 23898268; PubMed Central PMCID: PMC3724136.
Chaugny C, Simon J, Collin-Masson H, De Beauchęne M, Cabral D, Fagniez O, Veyssier-Belot C. [Vitamin B12 deficiency due to nitrous oxide use: unrecognized
cause of combined spinal cord degeneration]. Rev Med Interne. 2014 May;35(5):328-32. doi: 10.1016/j.revmed.2013.04.018. Epub 2013 Jun 14. French. PubMed PMID: 23773901.
Cheng HM, Park JH, Hernstadt D. Subacute combined degeneration of the spinal cord following recreational nitrous oxide use. BMJ Case Rep. 2013 Mar 8;2013.
pii: bcr2012008509. doi: 10.1136/bcr-2012-008509. PubMed PMID: 23476009; PubMed Central PMCID: PMC3618752.
Ghobrial GM, Dalyai R, Flanders AE, Harrop J. Nitrous oxide myelopathy posing as spinal cord injury. J Neurosurg Spine. 2012 May;16(5):489-91. doi:10.3171/2012.2.SPINE11532. Epub 2012 Mar 2. PubMed PMID: 22385084.
Probasco JC, Felling RJ, Carson JT, Dorsey ER, Niessen TM. Teaching NeuroImages: myelopathy due to B₁₂ deficiency in long-term colchicine treatment
and nitrous oxide misuse. Neurology. 2011 Aug 30;77(9):e51. doi:10.1212/WNL.0b013e31822c910f. PubMed PMID: 21876193.
Lin RJ, Chen HF, Chang YC, Su JJ. Subacute combined degeneration caused by nitrous oxide intoxication: case reports. Acta Neurol Taiwan. 2011 Jun;20(2):129-37. Review. PubMed PMID: 21739392.
Hathout L, El-Saden S. Nitrous oxide-induced B12 deficiency myelopathy: Perspectives on the clinical biochemistry of vitamin B12. J Neurol Sci. 2011 Feb
15;301(1-2):1-8. doi: 10.1016/j.jns.2010.10.033. Epub 2010 Nov 26. Review. PubMed PMID: 21112598.
Alt RS, Morrissey RP, Gang MA, Hoffman RS, Schaumburg HH. Severe myeloneuropathy from acute high-dose nitrous oxide (N2O) abuse. J Emerg Med. 2011
Oct;41(4):378-80. doi: 10.1016/j.jemermed.2010.04.020. Epub 2010 Jun 7. PubMed PMID: 20605391.
Richardson PG. Peripheral neuropathy following nitrous oxide abuse. Emerg Med Australas. 2010 Feb;22(1):88-90. doi: 10.1111/j.1742-6723.2009.01262.x. PubMedPMID: 20152009.
Wijesekera NT, Davagnanam I, Miszkiel K. Subacute combined cord degeneration: a rare complication of nitrous oxide misuse. A case report. Neuroradiol J. 2009
May 15;22(2):194-7. Epub 2009 May 15. PubMed PMID: 24207040.
Renard D, Dutray A, Remy A, Castelnovo G, Labauge P. Subacute combined degeneration of the spinal cord caused by nitrous oxide anaesthesia. Neurol Sci.
2009 Feb;30(1):75-6. doi: 10.1007/s10072-009-0013-2. Epub 2009 Jan 24. PubMed PMID: 19169627.
Jameson M, Roberts S, Anderson NE, Thompson P. Nitrous oxide-induced vitamin B(12) deficiency. J Clin Neurosci. 1999 Mar;6(2):164-6. PubMed PMID: 18639144.
Sethi NK, Mullin P, Torgovnick J, Capasso G. Nitrous oxide "whippit" abuse presenting with cobalamin responsive psychosis. J Med Toxicol. 2006 Jun;2(2):71-4. Review. PubMed PMID: 18072118; PubMed Central PMCID: PMC3550053.
Krajewski W, Kucharska M, Pilacik B, Fobker M, Stetkiewicz J, Nofer JR, Wronska-Nofer T. Impaired vitamin B12 metabolic status in healthcare workers
occupationally exposed to nitrous oxide. Br J Anaesth. 2007 Dec;99(6):812-8. Epub 2007 Oct 20. PubMed PMID: 17951609.
Wu MS, Hsu YD, Lin JC, Chen SC, Lee JT. Spinal myoclonus in subacute combined degeneration caused by nitrous oxide intoxication. Acta Neurol Taiwan. 2007
Jun;16(2):102-5. PubMed PMID: 17685135.
Singer MA, Lazaridis C, Nations SP, Wolfe GI. Reversible nitrous oxide-induced myeloneuropathy with pernicious anemia: case report and literature review. Muscle Nerve. 2008 Jan;37(1):125-9. PubMed PMID: 17623854.
Cohen Aubart F, Sedel F, Vicart S, Lyon-Caen O, Fontaine B. [Nitric-oxide triggered neurological disorders in subjects with vitamin B12 deficiency]. Rev Neurol (Paris). 2007 Mar;163(3):362-4. French. PubMed PMID: 17404524.
Ahn SC, Brown AW. Cobalamin deficiency and subacute combined degeneration after nitrous oxide anesthesia: a case report. Arch Phys Med Rehabil. 2005 Jan;86(1):150-3. PubMed PMID: 15641006.
Miller MA, Martinez V, McCarthy R, Patel MM. Nitrous oxide "whippit" abuse presenting as clinical B12 deficiency and ataxia. Am J Emerg Med. 2004 Mar;22(2):124. PubMed PMID: 15011232.
Waclawik AJ, Luzzio CC, Juhasz-Pocsine K, Hamilton V. Myeloneuropathy from nitrous oxide abuse: unusually high methylmalonic acid and homocysteine levels.
WMJ. 2003;102(4):43-5. Erratum in: WMJ. 2003;102(6):5. PubMed PMID: 12967021.
Ilniczky S, Jelencsik I, Kenéz J, Szirmai I. MR findings in subacute combined degeneration of the spinal cord caused by nitrous oxide anaesthesia--two cases.
Eur J Neurol. 2002 Jan;9(1):101-4. PubMed PMID: 11784385.
Barbosa L, Leal I, Timóteo AT, Matias T. [Acute megaloblastic anemia caused by inhalation of nitrous oxide in a patient with multiple autoimmune pathology]. Acta Med Port. 2000 Sep-Dec;13(5-6):309-12. Portuguese. PubMed PMID: 11234497.
Deleu D, Hanssens Y, Louon A. Nitrous oxide-induced cobalamin deficiency. Arch Neurol. 2001 Jan;58(1):134-5. PubMed PMID: 11176951.
McNeely JK, Buczulinski B, Rosner DR. Severe neurological impairment in an infant after nitrous oxide anesthesia. Anesthesiology. 2000 Dec;93(6):1549-50.
PubMed PMID: 11149458.
Felmet K, Robins B, Tilford D, Hayflick SJ. Acute neurologic decompensation in an infant with cobalamin deficiency exposed to nitrous oxide. J Pediatr. 2000 Sep;137(3):427-8. PubMed PMID: 10969273.
Marié RM, Le Biez E, Busson P, Schaeffer S, Boiteau L, Dupuy B, Viader F. Nitrous oxide anesthesia-associated myelopathy. Arch Neurol. 2000 Mar;57(3):380-2. PubMed PMID: 10714665.
Göthe CJ, Petersson G. [Nitrous oxide and cobalamin deficiency]. Lakartidningen. 1999 Dec 15;96(50):5609. Swedish. PubMed PMID: 10643221.
Lindstedt G. [Nitrous oxide can cause cobalamin deficiency. Vitamin B12 is a simple and cheap remedy]. Lakartidningen. 1999 Nov 3;96(44):4801-5. Review.
Swedish. PubMed PMID: 10584542.
Alarcia R, Ara JR, Serrano M, García M, Latorre AM, Capablo JL. [Severe polyneuropathy after using nitrous oxide as an anesthetic. A preventable disease?]. Rev Neurol. 1999 Jul 1-15;29(1):36-8. Spanish. PubMed PMID: 10528308.
Sesso RM, Iunes Y, Melo AC. Myeloneuropathy following nitrous oxide anesthaesia in a patient with macrocytic anaemia. Neuroradiology. 1999 Aug;41(8):588-90. PubMed PMID: 10447571.
Mayall M. Vitamin B12 deficiency and nitrous oxide. Lancet. 1999 May 1;353(9163):1529. PubMed PMID: 10232347.
Pema PJ, Horak HA, Wyatt RH. Myelopathy caused by nitrous oxide toxicity. AJNR Am J Neuroradiol. 1998 May;19(5):894-6. PubMed PMID: 9613506.
Beltramello A, Puppini G, Cerini R, El-Dalati G, Manfredi M, Roncolato G, Idone D, De Togni L, Turazzini M. Subacute combined degeneration of the spinal
cord after nitrous oxide anaesthesia: role of magnetic resonance imaging. J Neurol Neurosurg Psychiatry. 1998 Apr;64(4):563-4. PubMed PMID: 9576560; PubMed
Central PMCID: PMC2170040.
Horne DW, Holloway RS. Compartmentation of folate metabolism in rat pancreas: nitrous oxide inactivation of methionine synthase leads to accumulation of 5-methyltetrahydrofolate in cytosol. J Nutr. 1997 Sep;127(9):1772-5. PubMed PMID: 9278558.
Takács J. [N2O-induced acute funicular myelosis in latent vitamin B 12 deficiency]. Anasthesiol Intensivmed Notfallmed Schmerzther. 1996 Oct;31(8):525-8. German. PubMed PMID: 9019188.
Nestor PJ, Stark RJ. Vitamin B12 myeloneuropathy precipitated by nitrous oxide anaesthesia. Med J Aust. 1996 Aug 5;165(3):174. PubMed PMID: 8709889.
Rösener M, Dichgans J. Severe combined degeneration of the spinal cord after nitrous oxide anaesthesia in a vegetarian. J Neurol Neurosurg Psychiatry. 1996
Mar;60(3):354. PubMed PMID: 8609528; PubMed Central PMCID: PMC1073874.
Hadzic A, Glab K, Sanborn KV, Thys DM. Severe neurologic deficit after nitrous oxide anesthesia. Anesthesiology. 1995 Oct;83(4):863-6. Review. PubMed PMID: 7574068.
King M, Coulter C, Boyle RS, Whitby RM. Neurotoxicity from overuse of nitrous oxide. Med J Aust. 1995 Jul 3;163(1):50-1. PubMed PMID: 7609693.
Young PB, Kennedy S, Molloy AM, Scott JM, Weir DG, Kennedy DG. Effect of N2O treatment/vitamin B12 deficiency in pigs on tissue concentrations of odd-numbered, branched-chain fatty acids. Int J Vitam Nutr Res.1995;65(4):255-60. PubMed PMID: 8789622.
Louis-Ferdinand RT. Myelotoxic, neurotoxic and reproductive adverse effects of nitrous oxide. Adverse Drug React Toxicol Rev. 1994 Winter;13(4):193-206.Review. PubMed PMID: 7734639.
Flippo TS, Holder WD Jr. Neurologic degeneration associated with nitrous oxide anesthesia in patients with vitamin B12 deficiency. Arch Surg. 1993 Dec;128(12):1391-5. Review. PubMed PMID: 8250714.
Carmel R, Rabinowitz AP, Mazumder A. Metabolic evidence of cobalamin deficiency in bone marrow cells harvested for transplantation from donors given nitrous oxide. Eur J Haematol. 1993 Apr;50(4):228-33. PubMed PMID: 8500605.
Koblin DD, Tomerson BW, Waldman FM, Lampe GH, Wauk LZ, Eger EI 2nd. Effect of nitrous oxide on folate and vitamin B12 metabolism in patients. Anesth Analg. 1990 Dec;71(6):610-7. PubMed PMID: 2240633.
Koblin DD, Tomerson BW, Waldman FM. Disruption of folate and vitamin B12 metabolism in aged rats following exposure to nitrous oxide. Anesthesiology. 1990 Sep;73(3):506-12. PubMed PMID: 2393136.
van Achterbergh SM, Vorster BJ, Heyns AD. The effect of sepsis and short-term exposure to nitrous oxide on the bone marrow and the metabolism of vitamin B12 and folate. S Afr Med J. 1990 Sep 1;78(5):260-3. PubMed PMID: 2392722.
van der Westhuyzen J, Davis RE, Icke GC, Metz J. Tissue folates in fruit bats (Rousettus aegyptiacus) with nitrous oxide-induced vitamin B12 deficiency and neurological impairment. Br J Nutr. 1987 Nov;58(3):485-91. PubMed PMID:3120768.
Van de List C, Combs M, Schilling RF. Nitrous oxide and vitamin B12 deficiency interact adversely on rat growth. J Lab Clin Med. 1986 Oct;108(4):346-8. PubMed PMID: 3760674.
Koblin DD, Biebuyck JF. Is nitrous oxide a dangerous anesthetic for vitamin B12-deficient subjects? JAMA. 1986 Aug 8;256(6):716. PubMed PMID: 3723770.
Schilling RF. Is nitrous oxide a dangerous anesthetic for vitamin B12-deficient subjects? JAMA. 1986 Mar 28;255(12):1605-6. PubMed PMID: 3951096.
McLoughlin JL, Cantrill RC. Nitrous oxide induced vitamin B12 deficiency: measurement of methylation reactions in the fruit bat (Rousettus aegyptiacus).
Int J Biochem. 1986;18(2):199-202. PubMed PMID: 3949064.
Wilson SD, Horne DW. Effect of nitrous oxide inactivation of vitamin B12 on the levels of folate coenzymes in rat bone marrow, kidney, brain, and liver. Arch Biochem Biophys. 1986 Jan;244(1):248-53. PubMed PMID: 3947060.
van Tonder SV, Ruck A, van der Westhuyzen J, Fernandes-Costa F, Metz J. Dissociation of methionine synthetase (EC 2.1.1.13) activity and impairment of
DNA synthesis in fruit bats (Rousettus aegyptiacus) with nitrous oxide-induced vitamin B12 deficiency. Br J Nutr. 1986 Jan;55(1):187-92. PubMed PMID: 3663573.
van der Westhuyzen J, van Tonder SV, Gibson JE, Kilroe-Smith TA, Metz J.Plasma amino acids and tissue methionine levels in fruit bats (Rousettus aegyptiacus) with nitrous oxide-induced vitamin B12 deficiency. Br J Nutr. 1985 May;53(3):657-62. PubMed PMID: 4063293.
O'Leary PW, Combs MJ, Schilling RF. Synergistic deleterious effects of nitrous oxide exposure and vitamin B12 deficiency. J Lab Clin Med. 1985 Apr;105(4):428-31. PubMed PMID: 3981056.
van der Westhuyzen J, Metz J. Betaine delays the onset of neurological impairment in nitrous oxide-induced vitamin B-12 deficiency in fruit bats. J Nutr. 1984 Jun;114(6):1106-11. PubMed PMID: 6726473.
van der Westhuyzen J, Fernandes-Costa F, Metz J. Cobalamin inactivation by nitrous oxide produces severe neurological impairment in fruit bats : protection by methionine and aggravation by folates. Life Sci. 1982 Nov 1;31(18):2001-10. PubMed PMID: 7176808.
Lumb M, Perry J, Deacon R, Chanarin I. Urinary folate loss following inactivation of vitamin B12 by nitrous oxide in rats. Br J Haematol. 1982 Jun;51(2):235-42. PubMed PMID: 7082582.
Kondo H, Osborne ML, Kolhouse JF, Binder MJ, Podell ER, Utley CS, Abrams RS, Allen RH. Nitrous oxide has multiple deleterious effects on cobalamin metabolism and causes decreases in activities of both mammalian cobalamin-dependent enzymes in rats. J Clin Invest. 1981 May;67(5):1270-83. PubMed PMID: 6112240; PubMed Central PMCID: PMC370693.
Steinberg SE, Campbell C, Hillman RS. The effect of nitrous oxide-induced vitamin B12 deficiency on in vivo folate metabolism. Biochem Biophys Res Commun.
1981 Feb 27;98(4):983-9. PubMed PMID: 6164371.
McKenna B, Weir DG, Scott JM. The induction of functional vitamin B-12 deficiency in rats by exposure to nitrous oxide. Biochim Biophys Acta. 1980 Mar 20;628(3):314-21. PubMed PMID: 7370297.
Lumb M, Deacon R, Perry J, Chanarin I, Minty B, Halsey MJ, Nunn JF. The effect of nitrous oxide inactivation of vitamin B12 on rat hepatic folate.Implications for the methylfolate-trap hypothesis. Biochem J. 1980 Mar 15;186(3):933-6. PubMed PMID: 7396845; PubMed Central PMCID: PMC1161731.
Adornato BT. Nitrous oxide and vitamin B12. Lancet. 1978 Dec 16;2(8103):1318. PubMed PMID: 82831.
Deacon R, Lumb M, Perry J, Chanarin I, Minty B, Halsey MJ, Nunn JF. Selective inactivation of vitamin B12 in rats by nitrous oxide. Lancet. 1978 Nov
11;2(8098):1023-4. PubMed PMID: 82036.
Amess JA, Burman JF, Rees GM, Nancekievill DG, Mollin DL. Megaloblastic haemopoiesis in patients receiving nitrous oxide. Lancet. 1978 Aug12;2(8085):339-42. PubMed PMID: 79709.
Copyright © 2018 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited