
B12 Deficiency and Depression
After fatigue the most commonly reported symptom of vitamin B12 deficiency is depression.
Depression is common in conditions such as CFS, dementia and in many with autism.
Post Natal Depression/Post Partum Depression
Post Natal Depression/Post Partum Depression is extremely in women with reports of 1 in 10 or 1 in 5 women experiencing PND (Van Neil and Payne, 2020; Bagheri and Rostrami, 2021GTS). Over 50% of doctors fail to diagnose PND. If the depression extends to longer than 6 months it can often be accompanied by fatigue, with the result being the development of Chronic Fatigue Syndrome. This can have a devastating effect on the mother, and her enjoyment of her new born child or children. Even those that do diagnose the condition, fail to diagnose the cause, and so cannot effectively treat the condition. Interestingly, the risk factors for PND are similar to those for having a child with autism, and include, preterm delivery, preeclampsia, low birth weight, and behavioural disturbances in the baby (Van Neil and Payne, 2020), and is associated with a higher risk of maternal suicide (Shi etal, 2018). PND is also associated with impaired bonding between mother and child, poor development, marital discord, and infanticide (Wilkinson et al, 2017). Despite this, the standard of care (a curious misnomer) is NOT to screen for PND!! Recently an association between lower absolute levels of vitamin B12, and lower levels of functional B12 and post natal depression has been found (Dhiman et al, 2021; Ramadam, et al, 2022; Bodnar and Wisner, 2008)
Major Depressive Disorder
Major Depressive Disorder (MDD) at some time during the lifetime, is estimated to occur in at least 21% of individuals in the US, however its cause is not well understood (Maletic etal, 2023). The majority of doctors and psychiatrists believe that depression is caused by low serotonin levels, a theory that was first proposed in the 1960s and recent surveys suggest that over 80% of individuals with depression believe in the theory. The standard method of treatment has been the use of Selective Serotonin Reuptake Inhibitors (SSRIs) HOWEVER, recent a recent review has shown no evidence of low serotonin levels in depression (Moncrieff etal, 2022), and more recently Organic Acids tests of those with depression have shown exactly the opposite (Russell-Jones, 2022).
Using a standard symptom check-list of over 250 individuals with functional vitamin B12 deficiency, over 54% listed depression as a symptom.
Vitamin B12 Deficiency and Depression
Low levels of serum B12 and folate have been associated with low levels of vitamin B12 and folate (Khosravi etal, 2020).
The following text will describe the potential reason for why vitamin B12 deficiency is linked to depression.
You have two "happiness" neuropeptides, dopamine and serotonin. These two molecules, though, are also precursors for the production of nor-adrenalin, followed by adrenalin (epinephrine) and melatonin.
In vitamin B12 deficiency (more specifically methyl B12 deficiency), you cannot convert the precursors nor-adrenalin to adrenalin and serotonin to melatonin, but the body tries to drive these reactions by increasing the levels of both dopamine and serotonin (a Principle called Le Chatelier's Principle), hoping to get at least a little bit, and in some people the levels of serotonin, as measured by the breakdown product 5HIAA, are over 200 times the levels in normal individuals, and some long term very depleted people are even higher.
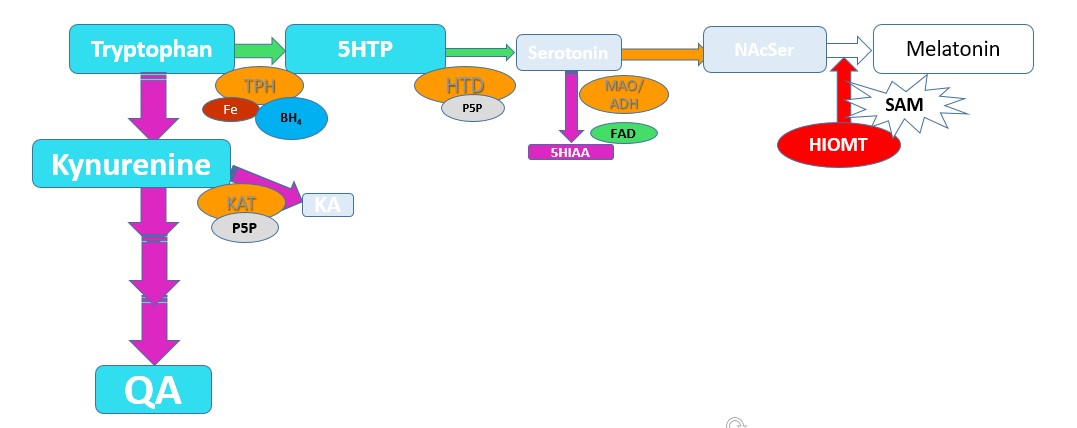
The final step in production of Melatonin is the methylation of N-Acetyl-Serotonin (NAcSer) by the enzyme HydroxyIndole-O-methyltransferase (HIOMT), which has an absolute requirement for S-Adenosylmethionine (SAM), a product of the methylation cycle (Axelrod and Weissbach 1960, Weissbach and Axelrod 1960).
Melatonin synthesis and SAM
In Methyl B12 deficiency, there is a greatly reduced production of SAM, and breakdown products of tryptophan, Kynurenic acid (KA) and Quinolinic acid (QA), as well as the breakdown product of Serotonin, 5-Hydroxyindoleacetic acid (5HIAA) start to accumulate and can be detected as elevated levels in urine.
Metabolites increased in SAM deficiency
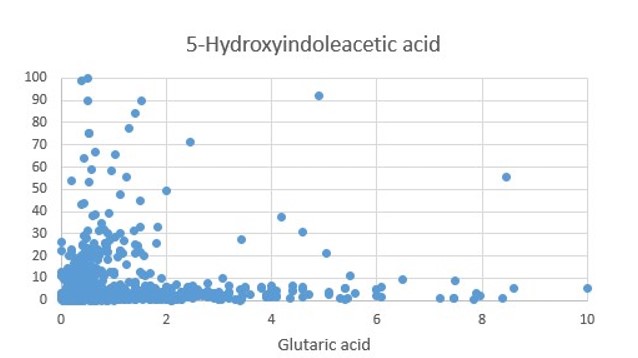
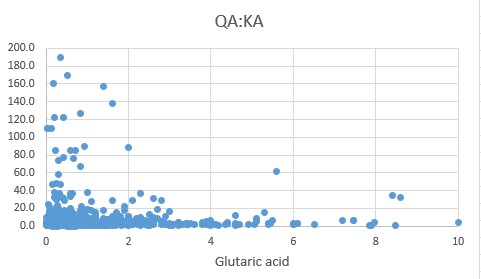
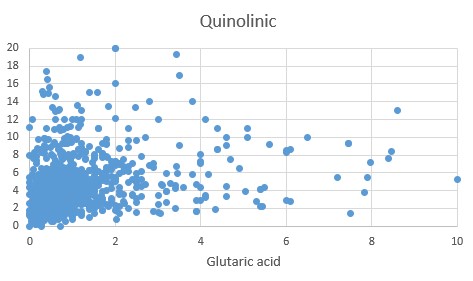
Increased amounts of QA, KA and 5HIAA in vitamin B12 deficiency are shown in the following scattergrams. Of particular note is the extremely elevated 5HIAA, the degradation product of serotonin, reflecting the highly elevated levels of serotonin produced in vitamin B12 deficiency. (Russell-Jones 2022)
Quinolinic Acid in B12 Deficiency
Kynurenic Acid in B12 Deficiency
5HIAA in B12 deficiency
The body though is very clever and so it turns off, or dims, the response to dopamine and serotonin, by reducing the numbers of receptors (the proteins or pores that detect the neuropeptides) for them - Receptor down-regulation, which eventually leads to depression in its own right. Depression is one of the most common symptoms of B12 deficiency, and in surveys, 53% of individuals with functional vitamin B12 deficiency report depression as a major symptom.
At this stage the body has a problem in that if you actually do get a stimulate that would cause you happiness, the stimulus doesn't work, a little like trying to see a firefly when all the lights are on, or trying to hear a pin-drop in a very noisy hall. You cannot detect either, due to the "white noise" and neither can the body detect the small increase that occurs when you do get a happy feeling. Eventually you compensate a bit for this and so are not "too depressed".
When you start to fix the B2 deficiency, one of the first things that is does is to start up a little bit of methylation, and then you start to convert the precusors, dopamine and serotonin to adrenalin and melatonin, and now you have a new problem. The levels of dopamine and serotonin drop rapidly, BUT, the receptors are now so few that they can't respond to the decreased levels of dopamine and serotonin, and so you feel even more depressed. This is one of the reasons why people who are on anti-depressants, such as SSRIs or SNRIs can't easily get off them, and why doctors don't suggest it just in case you can't cope. This would be more typical in major depressive disorder, but it can result in attempted suicide.
The body, though, eventually (and the active word is eventually) adapts and starts to turn up the number of receptors (Receptor up-regulation) in its quest to "find perpetual happiness". The trouble being that this takes a very long time, and so you have to do be very methodical and gradually reduce the dose, potentially by as little as 1% per day. This is the same advice that doctors suggest for coming off antidepressants or other addictive drugs. Curiously, the B12 deficient person, is just like a person on SSRIs is addicted to their own-overproduction of serotonin and dopamine. Not that you generally hear this discussed like this.
Studies on use of high dose 5-methyl-folate support the concept that in prolonged depression functional vitamin B12 may be the issue (Maletic etal, 2023). Unfortunately the authors looked neither at functional vitamin B2 sufficiency, nor functional B12 sufficiency.
Functional Vitamin B12 Deficiency due to functional B2 deficiency
Functional vitamin B2 deficiency, which can be the result of deficiency in Iodine, Selenium and/or Molybdenum will also cause functional B12 deficiency, however the consequences on the levels of neurotransmitter metabolites are different. Hence as the amount of active B2, as FAD decreases, more and more serotonin is synthesized, but due to Methyl B12 deficiency, it accumulates and is degraded by the FAD-dependent enzyme MAO, leading to very high levels of the degradation product 5HIAA. In functional B2 deficiency due to lack of Iodine or Selenium, there is lower synthesis of FAD, and so the degradation product 5HIAA rapidly declines. Further, this deficiency then causes a deficiency in the synthesis of Pyridoxal-5-phosphate (P5P) and so synthesis of serotonin is blocked, and the levels of QA go up. Degradation of Kynurenine to KA is also dependent upon a P5P-dependent enzyme, and so as the deficiency increases the ratio of QA:KA increases. Yet, as can be seen levels of QA keep increasing as the functional B2 deficiency increases.
Vitamin B12 Deficiency, Drug Treatment and Depression
The most common treatments for depression are SSRIs, indicating that it is the serotonin system that is being incorrectly treated. SSRIs are highly addictive and include drugs such as Fluoxitene, Lexapro, Zooloft, Prozac, Paxil, Celexa, Luvox, Paxil, Brisdelle, etc. Given that the market for antidepressants is $4 billion, it is not in the drug companies best interests to test for vitamin B12 deficiency. Further, prolonged treatments usually require a psychiatrist, at over $250 per visit. Hence it is not in the psychiatrists best interests to test for B12 deficiency in the patients.
One can see from the graphs above, that treatment for plain B12 deficiency, would result in higher levels of melatonin, but would also result in rapid reduction in the amount of serotonin, potentially leading to increased anxiety, depression, suicidal tendencies, fear, anxiety, irritability, agitation, etc.
In contrast, if the functional vitamin B12 deficiency is due to Iodine, Selenium and Molybdenum deficiency, then as the deficiency is reduced, there potentially would be a sudden rise firstly in FMN, with concomitant production of P5P, leading to a sudden increase in serotonin, which would persist until the activation of MAO, at which time there would be an increase in 5HIAA. Further treatment of the functional B2 deficiency, when combined with Methyl B12, would then lead to a rapid drop in serotonin (once again leading to increased anxiety, depression, suicidal tendencies, fear, irritability and agitation), and lead to symptoms synonymous with SSRI withdrawal.
This is further compounded by what is happening to the receptors for serotonin.
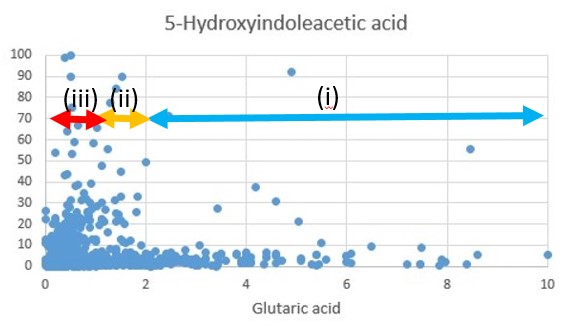
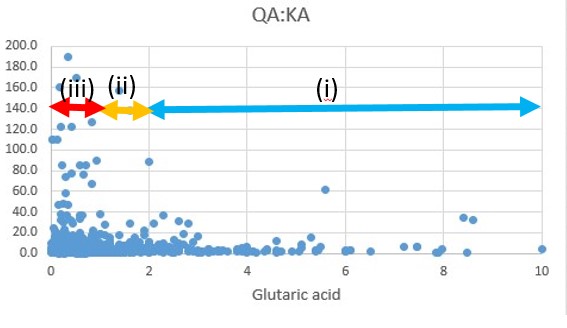
i) In extreme Iodine/Selenium deficiency, there is very little serotonin produced. This will then result in very elevated levels of serotonin receptor expression. This is predominantly seen as glutaric acid levels rise above 1.5. If at that stage I/Se are introduced too quickly, there is a sudden increase in the rate of conversion of 5HTP to serotonin, and as the enzyme MAO requires FAD, it is unable to 'cope" with this rise and so you have a combination of very high serotonin levels and very high serotonin receptor levels resulting in some extreme serotonin overload symptoms.
ii) As Iodine and Selenium become replete, there is a gradual increase in the rate of serotonin synthesis, and the QA:KA ratio decreases, and there is gradual decrease in the numbers of serotonin receptors, until the levels of receptors gets very low, to balance the increased amount of serotonin that is produced.
iii) At this stage if Molybdenum is very low, then degradation of serotonin is very slow, but if Molybdenum is introduced, there can be a rapid conversion of serotonin to 5HIAA, whose levels can rise to exceedingly high levels. There is still a serotonin over-load.
iv). Once I/Se/Mo are replete, there is still a high production of serotonin, with low serotonin receptor numbers, if Methyl B12 is now introduced there is a rapid conversion of serotonin to melatonin. Serotonin receptor numbers are very low, serotonin becomes very low and now there are symptoms of serotonin deficiency, such as increased anxiety, depression, suicidal tendencies, fear, irritability and symptoms of similar to SSRI withdrawal occur.
Treatment
Depression is an extremely common disorder with as much as 10% of the population above 12 years of age being affected. in the US the cost of treatment of depression is over $70 billion. Much of the treatment of depression is based on the use of anti-depressants with the antidepressant market projected to reach US$30.59 by 2029. Much of the treatment revolves around the mis-guided notion that the person with depression is NOT making sufficient dopamine and/or serotonin, and so involves the use of SSRIs, SNRIs and TCA. Given the size of the market it is highly unlikely that one could convince the drug companies, that actually the problem is due to over-production of dopamine and serotonin, due ot functional B12 deficiency, with resultant receptor down-regulation. A somewhat "unfortunate truth" for the pharmaceutical industry.
Treatment resistant depression
The data on the lack of production of serotonin would explain Treatment Resistant Depression. In this case, persons who are Iodine or Selenium deficient, are not making serotonin, and so treatment options using SSRIs, or SNRIs will be unsuccessful. Treatment Resistant Depression has been quoted as representing up to 50% of all cases of depression. According to the World Health Organization (WHO), MDD is the single largest contributor to loss of healthy life. the majority of individuals with MDD are inadequately responsive to first‐line treatments. Moreover, a substantial proportion of them fail multiple antidepressant interventions, resulting in what is described as treatment‐resistant depression (TRD) (McIntyre etal, 2023). Associative conditions for TRD are diabetes, obesity and CVD, all of which are associated with low functional vitamin B2.
Treatment with Antipyschotics
Even a preliminary comparison to the processes outlined above, quickly draws similarities between treatment of depression and the use of highly addictive anti-psychotic medications such as Tiotthixine, pimozide, ueiapnie, chlorpromazine, clozapine, and fluphenzaine. The action of these drugs involves the inhibition of different receptors, including 5-HT (serotonin), dopaminergic, histaminergic, and adrenergic receptors, all of which are over-stimulated in Methyl B12 deficiency. Withdrawal symptoms are compensurate with this including insomnia (lack of melatonin), anxiety and depression (Storck et al, 2024).
Given that SSRIs are used to treat a range of conditions from depression, anxiety, OCD, panic disorder, severe phobias, PTSD, etc, one could assume that they have similar mechanisms to that outlined for depression. Drugs include Zooloft, Lexapro, Celexa, Prosac, Brisdelle, Paxil, etc. The current market is over US$150 billion, and one can assume that it is definitely NOT in the best interests of the drug companies and the psychiatrists, who charge $300-650 per visit, and who are urging patients to see them one or two times per week, to be made aware that the majority of these conditions are due to simple nutritional deficiency(ies).. It is clear from the literature that many experts in the field do not have a clue (Fuentes-Claramonte etal, 2024; Wang et al, 2022; Prata et al, 2014; Goff et al, 2016; Mirzakhanian et al, 2014; Bhatia and Singh, 2015). This is despite tell tale markers such as elevated homocysteine (Moradi et al, 2021; Bremner et al, 2021; Almeida et al, 2008_ elevated folate (Bottiglieri et al, 2005; Khosravi et al, 2020)
Other signs of Vitamin B12 Deficiency in Adults
There are many neuropsychiatric symptoms associated with functional vitamin B12 deficiency, including, depression, anxiety, psychosies, dementia, delirium, apathy, agitation, impraired concentration, insomnia, persecutory delusions, auditory and visual hallucinations, and disorganized thought processes.
References
Van Niel MS, Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May;87(5):273-277. doi: 10.3949/ccjm.87a.19054. PMID: 32357982.
Shi P, Ren H, Li H, Dai Q. Maternal depression and suicide at immediate prenatal and early postpartum periods and psychosocial risk factors. Psychiatry Res. 2018 Mar;261:298-306. doi: 10.1016/j.psychres.2017.12.085. Epub 2018 Jan 3. PMID: 29331710.
Bagheri P, Rostami M. Postpartum depression and suicide in Iran. Womens Health (Lond). 2021 Jan-Dec;17:17455065211043994. doi: 10.1177/17455065211043994. PMID: 34623208; PMCID: PMC8504209.
Wilkinson A, Anderson S, Wheeler SB. Screening for and Treating Postpartum Depression and Psychosis: A Cost-Effectiveness Analysis. Matern Child Health J. 2017 Apr;21(4):903-914. doi: 10.1007/s10995-016-2192-9. PMID: 27832444; PMCID: PMC5380488.
Khosravi M, Sotoudeh G, Amini M, Raisi F, Mansoori A, Hosseinzadeh M. The relationship between dietary patterns and depression mediated by serum levels of Folate and vitamin B12. BMC Psychiatry. 2020 Feb 13;20(1):63. doi: 10.1186/s12888-020-2455-2. PMID: 32054533; PMCID: PMC7020545.
Ramadan EF, Grisdale M, Morais M. Maternal Vitamin B12 Levels During Pregnancy and Their Effects on Maternal Neurocognitive Symptoms: A Systematic Review. J Obstet Gynaecol Can. 2022 Apr;44(4):390-394.e3. doi: 10.1016/j.jogc.2021.11.017. Epub 2021 Dec 16. PMID: 34921998.
Bodnar LM, Wisner KL. Nutrition and depression: implications for improving mental health among childbearing-aged women. Biol Psychiatry. 2005 Nov 1;58(9):679-85. doi: 10.1016/j.biopsych.2005.05.009. Epub 2005 Jul 25. PMID: 16040007; PMCID: PMC4288963.
Russell-Jones 2022 Vitamin B12 Deficiency and Depression: What is the mechanism PDF
Moncrieff, J., Cooper, R.E., Stockmann, T.
et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry (2022). https://doi.org/10.1038/s41380-022-01661-0Dhiman P, Pillai RR, Wilson AB, Premkumar N, Bharadwaj B, Ranjan VP, Rajendiran S. Cross-sectional association between vitamin B12 status and probable postpartum depression in Indian women. BMC Pregnancy Childbirth. 2021 Feb 17;21(1):146. doi: 10.1186/s12884-021-03622-x. PMID: 33596868; PMCID: PMC7890831.
Maletic V, Shelton R, Holmes V. A review of l-methylfolate as adjunctive therapy in the treatment of major depressive disorder. Prim Care Companion CNS Disord. 2023;25(3):22nr03361
McIntyre RS, Alsuwaidan M, Baune BT, Berk M, Demyttenaere K, Goldberg JF, Gorwood P, Ho R, Kasper S, Kennedy SH, Ly-Uson J, Mansur RB, McAllister-Williams RH, Murrough JW, Nemeroff CB, Nierenberg AA, Rosenblat JD, Sanacora G, Schatzberg AF, Shelton R, Stahl SM, Trivedi MH, Vieta E, Vinberg M, Williams N, Young AH, Maj M. Treatment-resistant depression: definition, prevalence, detection, management, and investigational interventions. World Psychiatry. 2023 Oct;22(3):394-412. doi: 10.1002/wps.21120. PMID: 37713549; PMCID: PMC10503923.
Storck W, de Laportalière TT, Yrondi A, Javelot H, Berna F, Montastruc F. Withdrawal syndrome after antipsychotics discontinuation: an analysis of the WHO database of spontaneous reports (Vigibase) between 2000 and 2022. Psychopharmacology (Berl). 2024 Jun;241(6):1205-1212. doi: 10.1007/s00213-024-06554-4. Epub 2024 Feb 20. PMID: 38376511.
Fuentes-Claramonte P, Estradé A, Solanes A, Ramella-Cravaro V, Garcia-Leon MA, de Diego-Adeliño J, Molins C, Fung E, Valentí M, Anmella G, Pomarol-Clotet E, Oliver D, Vieta E, Radua J, Fusar-Poli P. Biomarkers for Psychosis: Are We There Yet? Umbrella Review of 1478 Biomarkers. Schizophr Bull Open. 2024 Aug 30;5(1):sgae018. doi: 10.1093/schizbullopen/sgae018. PMID: 39228676; PMCID: PMC11369642.
Wang B, Zartaloudi E, Linden JF, Bramon E. Neurophysiology in psychosis: The quest for disease biomarkers. Transl Psychiatry. 2022 Mar 11;12(1):100. doi: 10.1038/s41398-022-01860-x. PMID: 35277479; PMCID: PMC8917164.
Prata D, Mechelli A, Kapur S. Clinically meaningful biomarkers for psychosis: a systematic and quantitative review. Neurosci Biobehav Rev. 2014 Sep;45:134-41. doi: 10.1016/j.neubiorev.2014.05.010. Epub 2014 May 27. PMID: 24877683.
Goff DC, Romero K, Paul J, Mercedes Perez-Rodriguez M, Crandall D, Potkin SG. Biomarkers for drug development in early psychosis: Current issues and promising directions. Eur Neuropsychopharmacol. 2016 Jun;26(6):923-37. doi: 10.1016/j.euroneuro.2016.01.009. Epub 2016 Mar 19. PMID: 27005595.
Mirzakhanian H, Singh F, Cadenhead KS. Biomarkers in psychosis: an approach to early identification and individualized treatment. Biomark Med. 2014;8(1):51-7. doi: 10.2217/bmm.13.134. PMID: 24325224; PMCID: PMC6984197.
Moradi F, Lotfi K, Armin M, Clark CCT, Askari G, Rouhani MH. The association between serum homocysteine and depression: A systematic review and meta-analysis of observational studies. Eur J Clin Invest. 2021 May;51(5):e13486. doi: 10.1111/eci.13486. Epub 2021 Jan 22. PMID: 33423269.
Bremner JD, Goldberg J, Vaccarino V. Plasma homocysteine concentrations and depression: A twin study. J Affect Disord Rep. 2021 Apr;4:100087. doi: 10.1016/j.jadr.2021.100087. Epub 2021 Jan 16. PMID: 34414386; PMCID: PMC8372975.
Almeida OP, McCaul K, Hankey GJ, Norman P, Jamrozik K, Flicker L. Homocysteine and depression in later life. Arch Gen Psychiatry. 2008 Nov;65(11):1286-94. doi: 10.1001/archpsyc.65.11.1286. PMID: 18981340.
Bottiglieri T. Homocysteine and folate metabolism in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2005 Sep;29(7):1103-12. doi: 10.1016/j.pnpbp.2005.06.021. PMID: 16109454.
Khosravi M, Sotoudeh G, Amini M, Raisi F, Mansoori A, Hosseinzadeh M. The relationship between dietary patterns and depression mediated by serum levels of Folate and vitamin B12. BMC Psychiatry. 2020 Feb 13;20(1):63. doi: 10.1186/s12888-020-2455-2. PMID: 32054533; PMCID: PMC7020545.
Bhatia P, Singh N. Homocysteine excess: delineating the possible mechanism of neurotoxicity and depression. Fundam Clin Pharmacol. 2015 Dec;29(6):522-8. doi: 10.1111/fcp.12145. Epub 2015 Sep 17. PMID: 26376956.
Sites on depression in the young
http://prp.jasonfoundation.com/facts/youth-suicide-statistics/
https://afsp.org/about-suicide/suicide-statistics/
https://afsp.org/about-suicide/suicide-statistics/
Support sites for treatment of depression
https://www.beyondblue.org.au/
Spoke to a Bloke | Men's Mental Health | Registered Charity
Copyright © 2018 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited