Elevated serum Vitamin B12 and Cancer
-
Elevated serum vitamin B12 has been found with certain cancers.
-
Vitamin B12-labelled imaging agents can be used successfully to image primary and secondary cancers
-
Potentially the presence or re-appearance of cancer could be monitored by measuring serum vitamin B12
-
Apart from vitamin B12, there is evidence of increased uptake of riboflavin, folate, and/or biotin into many cancers
-
Paradoxically high levels of ferritin can also be a marker of the presence of cancer
-
Elevated Apolipoprotein A and Apo B have been associated with some cancers
More recently elevated B12 levels have been associated with a poorer
prognosis following
treatment for cancer (Geissbühler
etal, 2000; Oh, etal, 2018;
Aloreidi and Zamulko, 2018;
Lin etal, 2010). The higher
the B12, the poorer the
prognosis. We have not been
able to find any study where
the authors have "looked at"
metabolic markers that one
would ascribe to functional
B2 deficiency, and compared
it to the elevated B12
levels in these cancer
studies. Studies on gastric
cancer have suggested that
the cancers themselves
over-produce haptocorrin (R
Binder), and hence elevated
serum Hc-B12 may be
indicative of prognosis (Wakatsuki
etal, 1989; Lee etal, 2017;
Waxman etal, 1977; Kane etal,
1978; Paradinas etal, 1982;
Arendt et al, 2013; 2016;
Takahashi et al, 2013).
Elevations of serum B12 have
also been found in cats with
neoplasms (Trehy etal,
2014). Extreme levels
of Hc-B12 (>18,000 pg/m B12)
have been found in some
metastatic cancers (Carmel,
1975) and may persist for
long after the cancer has
been treated, potentially
indicating the presence of
metastases (Lacombe etal,
2021). Studies by
Russell-Jones and co-workers
have shown that many cancers
over-express receptors
involved in vitamin B12
uptake, including breast
cancer. Elevated serum B12
has also been associated
with an increased risk of
cancer (Amado-Garzon
et al, 2024; Liu et al,
2024; Haghighat et al,
2023;
Matejcic et al, 2017; Kim et
al, 2017;
Essén et al, 2019;
Sottotetti et al,
2024;
Naushad
et al, 2014; Gimsing et al,
1987;
Pirouzpanah et al, 2014;
Collins et al, 2000).
Elevated B12 and Cancer
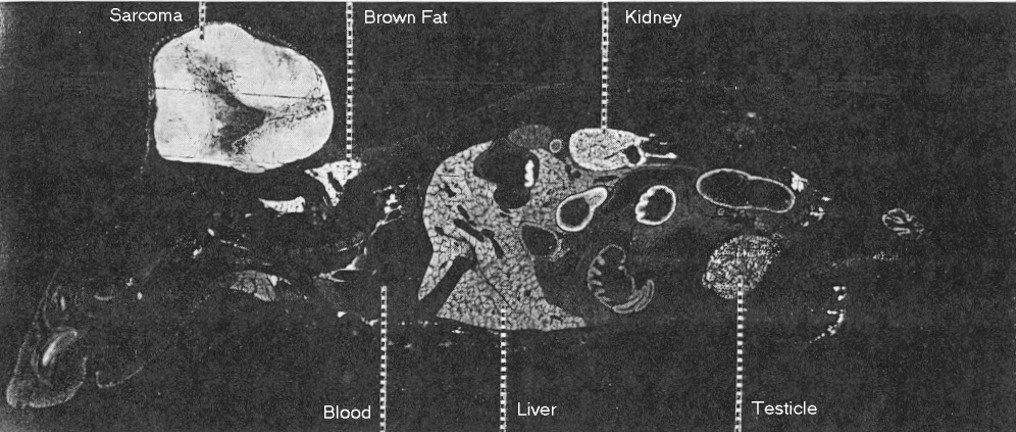
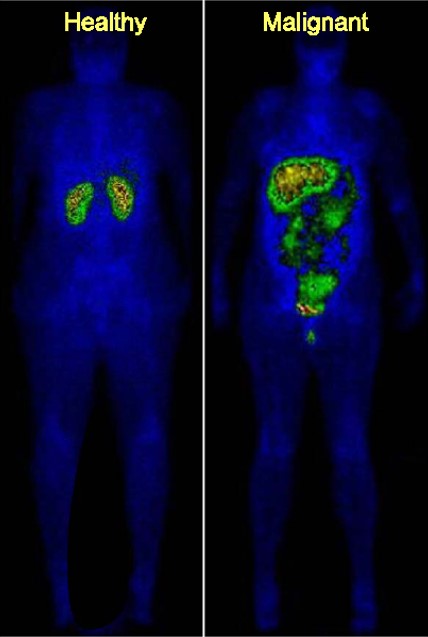
Vitamin B12 has been used as a targeting agent to image various tumours in vivo
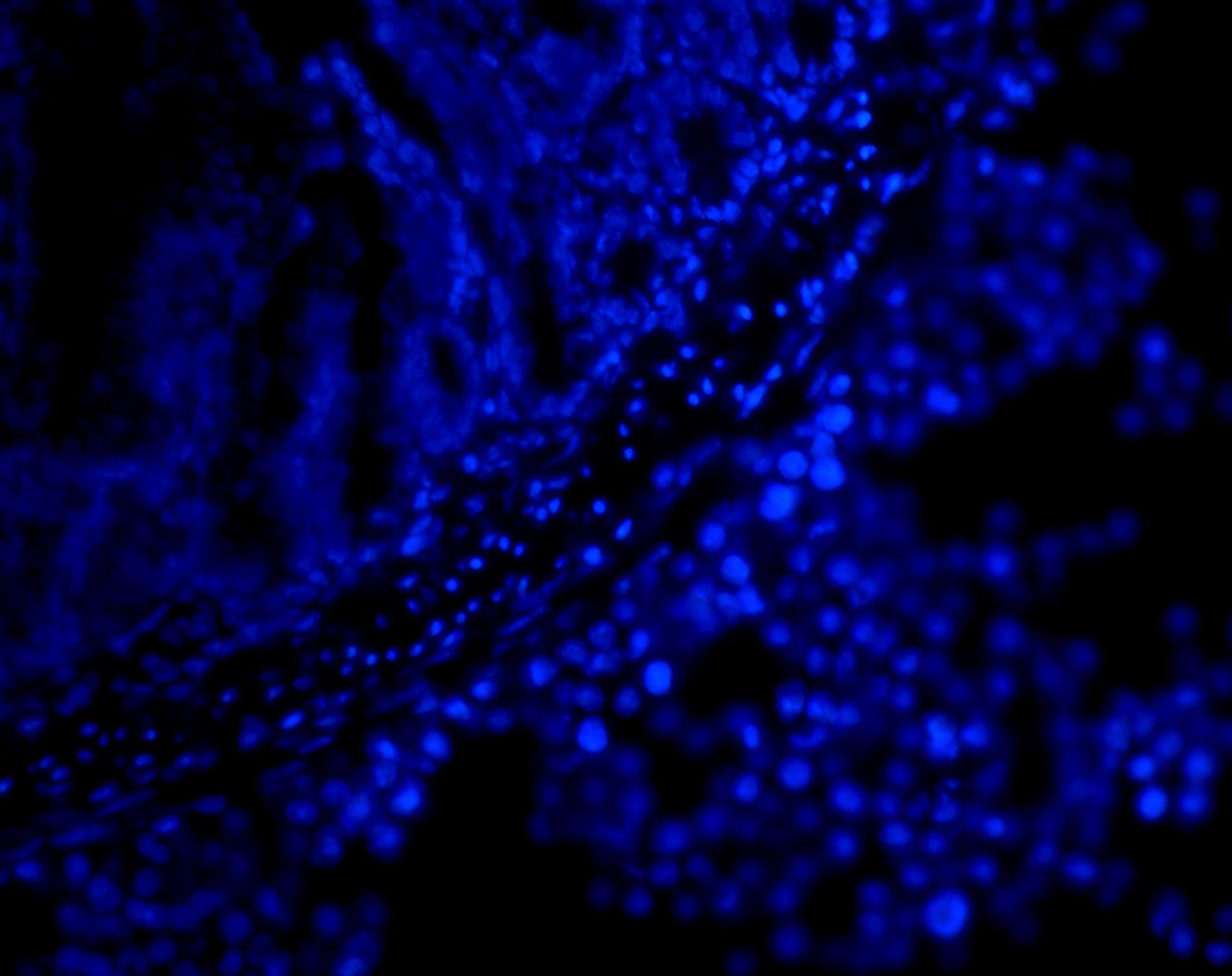
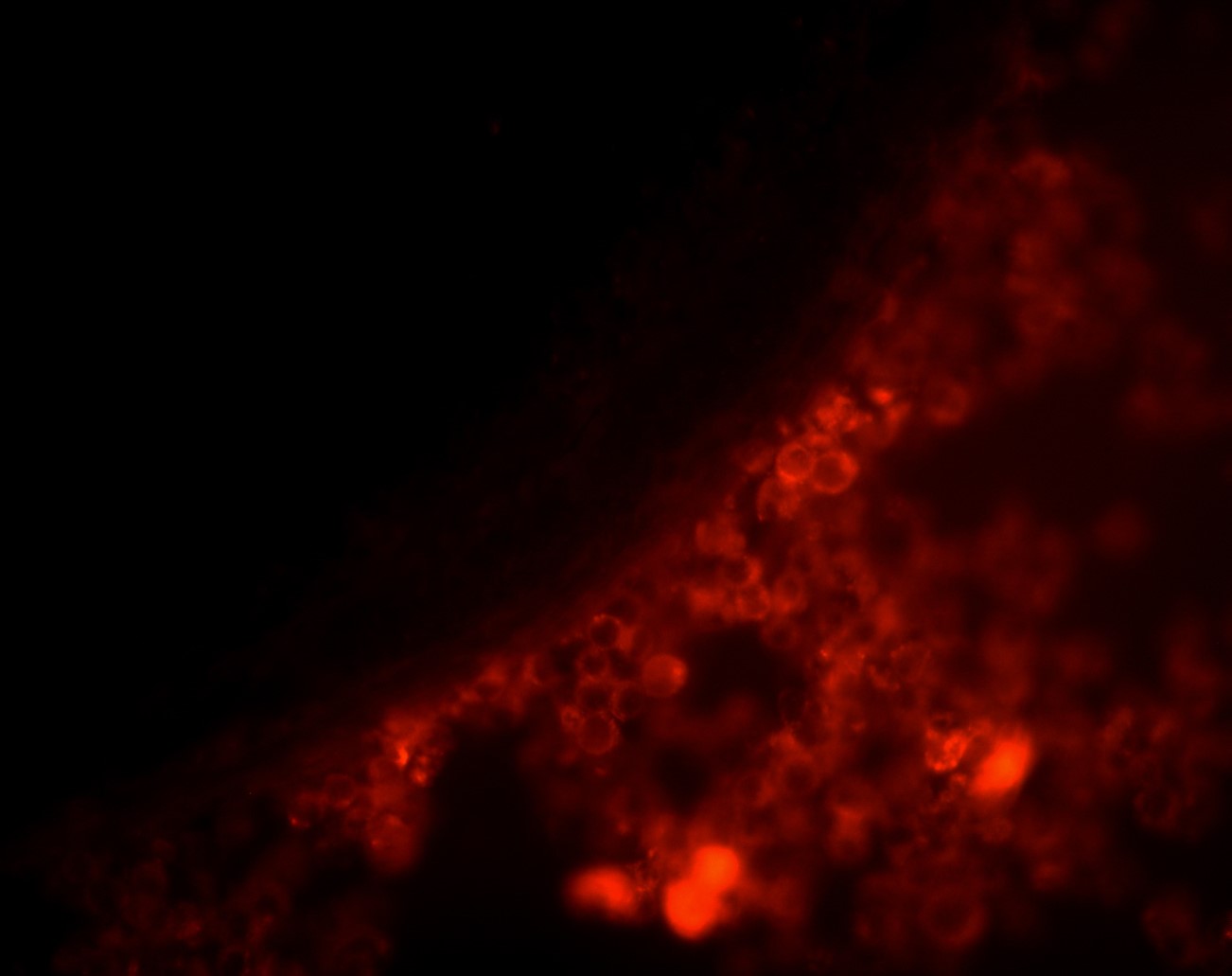
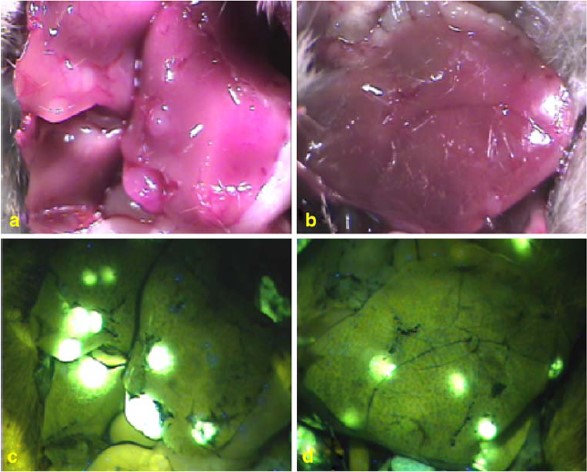
Vitamin B12-targeted
Rhodamine-labelled polymers have been used to image tumour metastases (top panel BisB nuclear staining of gut wall, middle panel BisB+B12-Rho-HPMA, lower panel B12-Rho-HPMA)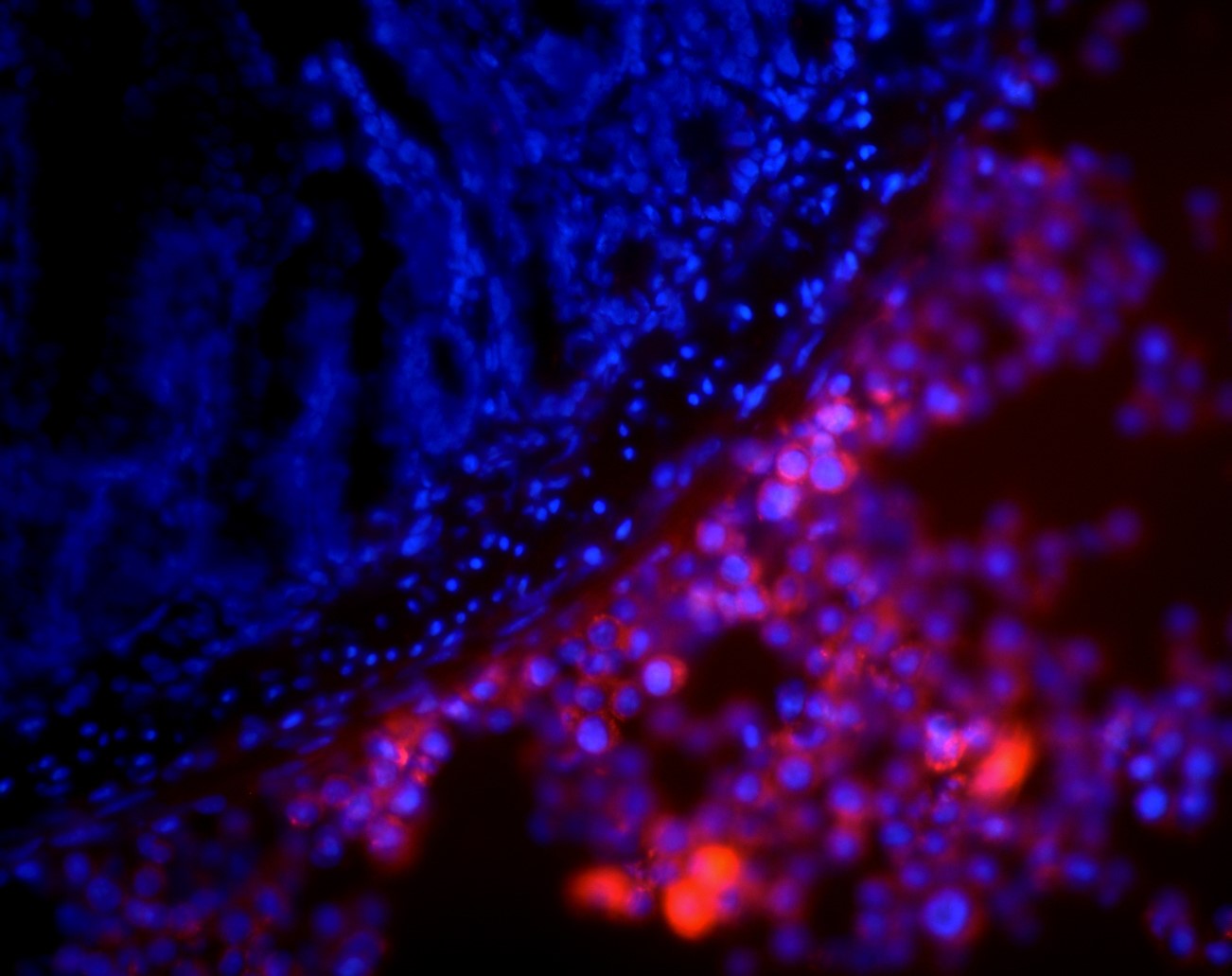
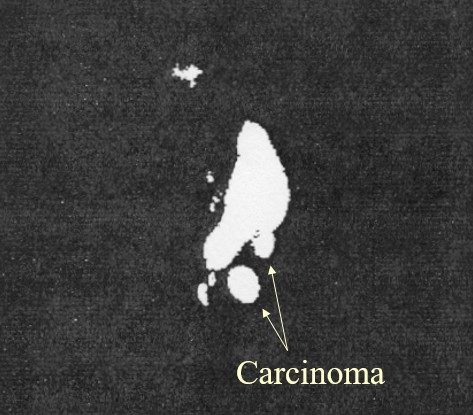
Radionucleotide labelling of cat mammary Carcinoma (AdenosylCbl-b-DTPA-Tc-99m iv)
Floyd and co-workers have used 131-I-Cbl to image a mouse sarcoma
Measurement of Serum B12, what does it mean?
In order to understand the data, and in order to stop the hysteria that may result from the concept that elevated B12 may be associated with cancer, one has to firstly understand what measurement of vitamin B12 in serum actually means.
Hence, Serum vitamin B12 is a measurement of circulating vitamin B12 that is bound by a vitamin B12 binding protein. There are two main binding proteins Haptocorrin and Transcobalamin. Hence serum vitamin B12 DOES NOT REPRESENT free unbound vitamin B12, it represents some form of cobalamin that is trapped in the body and is not filtered out by the kidney because it is bound to either Haptocorrin, or Transcobalamin. The incorrectly named Active B12 test, measured some form of cobalamin bound to Transcobalamin. In fact the more inactive B12 that is around the higher the values for both serum and inactive B12 are. In the case of elevated serum vitamin B12, due to the presence of cancer, the cancer cells themselves have been shown to secrete either binding protein, in an attempt to sequester vitamin B12 either from the diet, the liver or from supplementation. This the cancer will do, regardless of the amount of vitamin B12 supplemented or ingested. Logically, the lower the vitamin B12, the greater the expression of the vitamin B12 binding proteins. Since functional vitamin B12 deficiency can occur at any serum level, so too can "relatively" elevated vitamin B12. Hence the measurement of serum vitamin B12 should be done in comparison to levels before or after identification or treatment of cancer.
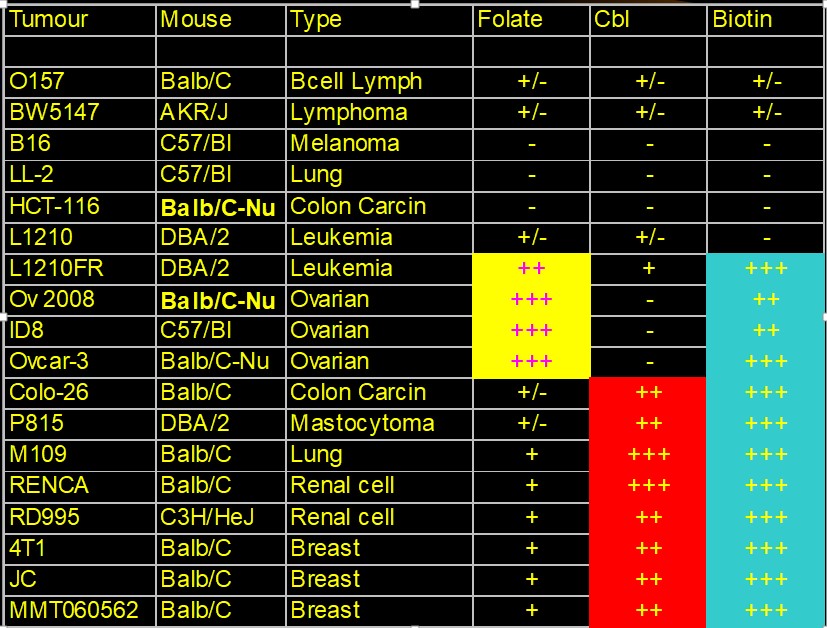
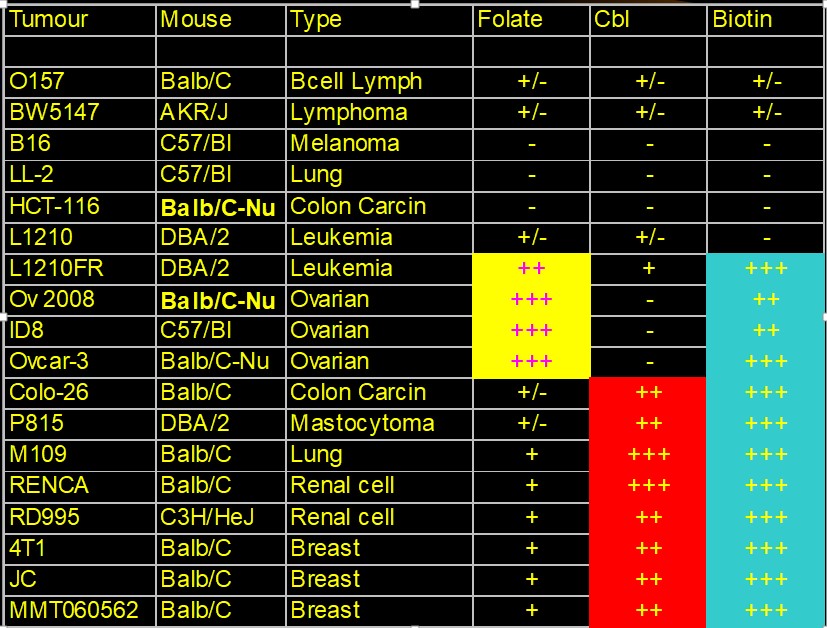
Folate targeting to Cancers
Several different types of cancers have been shown to have increased uptake of
folate (III-In-DTPA folate imaging)
-
Folate imaging has
been found to successfully detect metastatic cancers (Sega and Low 2008)
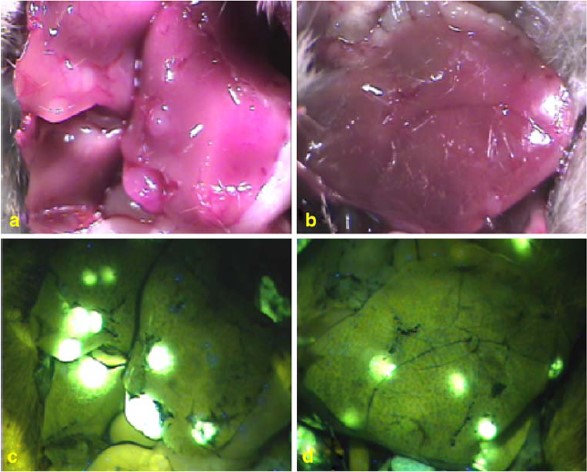
Biotin targeting to Cancers
Many cancers have also been found to have
greatly increased uptake of biotin (Russell-Jones et al, 2002, 2004, 2008), with
many have dual uptake of vitamin B12 and biotin, or folate and biotin)
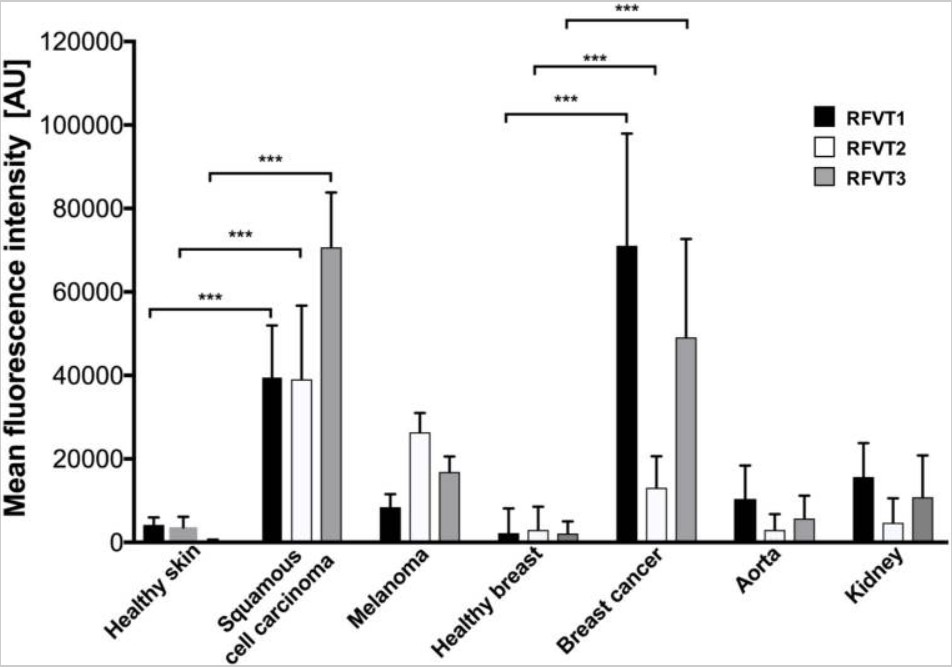
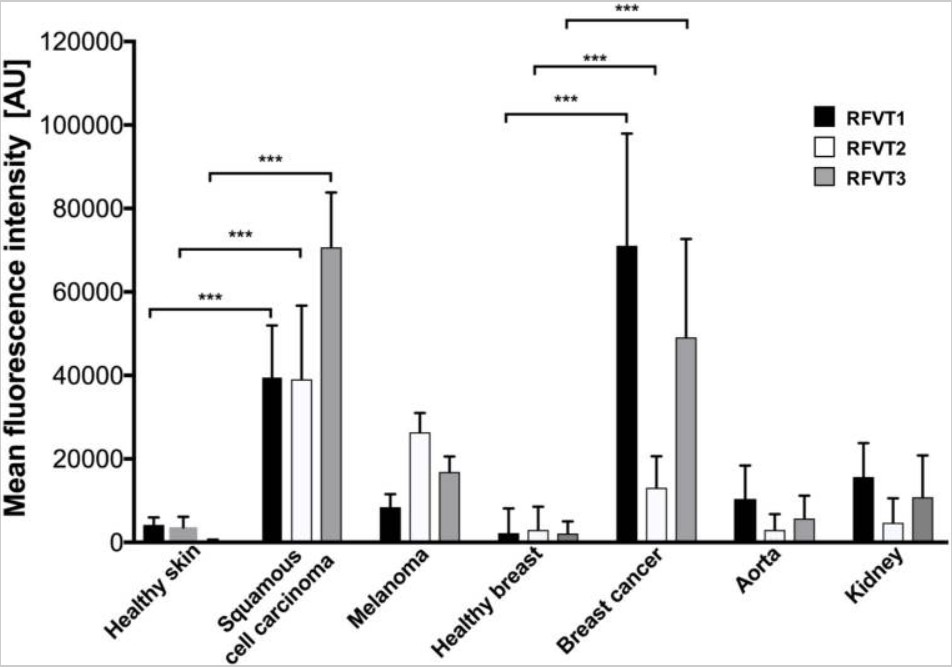
Riboflavin targeting to Cancers
More recently, riboflavin has also been
found to target several tumours, and there are reports of elevated Riboflavin
Carrier Protein being associated with pancreatic cancer (Paragomi
et al, 2023). RIboflavin seems to play a dual role in cancers, in low riboflavin
there is an increased risk
of some cancers (Long et al, 2021; Yu et al, 2016), possibly due to its role in
maintaining the activity of MTHFR and MTRR and the methylation cycle. In a
similar fashion to the elevated serum B12 in some cancers, elevated serum
riboflavin has been seen in colorectal cancer (Ma et al, 2023; Xu et al, 2022),
Levels of the riboflavin carrier protein (RCP) are 3 to 4 times normal in many cases
of breast and other cancers (Karande et al, 2001;
Darguzyte
et al, 2020). Riboflavin uptake is greatly enhanced in some tumour cells (Bartmann
et al, 2019). Riboflavin supplementation has been shown to increase cancer cell
proliferation, invasion and migration, and inhibition of of flavin-containing
enzymes arrested tumor growth (Yang et al, 2013; Ozsvari et al, 2017).
Rao
and coworkers (1999) found that serum
RCP
levels were significantly elevated in women with breast cancer (
6.06
+/- 7.27
ng/ml)
as compared with control subjects [0.70 +/- 0.19
ng/ml), Elevated
serum RCP
of > or = 1.0 ng/ml
was highly predictive of the presence of breast cancer, detecting 88% of tumors
in stages I-II and 100% of tumors in stages III-IV. Significantly
elevated RCP was also found in hepatacellular carcinoma (Rao et al, 2006), where
mean
serum RCP levels in HCC were
21.75+/-14.66ng/m, significantly higher than controls (0.73+/-0.25ng/ml).
Riboflavin has also been shown to have an inhibitory role in some cancer, with
levels of serum riboflavin lower in patients with
esophageal cancer (Bao et al,
2013)
Measurement of Serum riboflavin, what does it
mean?
In order to
understand the data, and in order to stop the hysteria that may result from the
concept that elevated riboflavin may be associated with cancer, one has to
firstly understand what measurement of vitamin B2 in serum actually means.
Hence, Serum vitamin B2 is a measurement of circulating
vitamin B2 that is either free, or is bound by a vitamin B2 binding protein.
In the case of elevated serum vitamin B2, due to the presence of cancer, the
cancer cells themselves have been shown to secrete a riboflavin binding protein,
in an attempt to sequester vitamin B2 either from the diet, the liver or from
supplementation. This the cancer will do, regardless of the amount of vitamin B2
supplemented or ingested. Logically, the lower the vitamin B2, the greater the
expression of the vitamin B2 binding proteins.
Since functional
vitamin B2 deficiency can occur at any serum level, so too can "relatively"
elevated vitamin B2. Hence the measurement of serum vitamin B2 should be done in
comparison to levels before or after identification or treatment of cancer.
Associated Factors - Apolipoproteins
Elevations in Apoliproteins have been
found to be associated with several cancers. ApoB, and ApoA have been shown to
have potential as diagnostic markers (Zhou and Luo, 2020)
Ferritin
Ferritin is differentially over-expressed in tissues from multiple malignancies,
including: hepatocellular carcinoma [46], [47], Hodgkin's lymphoma [48], breast
cancer [49], [50], [51], [52], [53], and pancreatic cancer [50]
Relevance of the elevated serum markers
There is strong evidence to suggest that
the treatment of various cancers could be followed by monitoring the serum
markers. Potentially they could be used in the initial diagnosis. There is some
debated about what to do, if you find the elevated markers, whether to
supplement or not. Evidence suggests that the reason for the elevated markers
was some sort of nutritional deficiency in the first. This then resulted in
lower methylation and thereby poorer control of oncogene expression.
Unfortunately, very, very clinicians know of the associations not do National
Cancer bodies such as the Cancer Council of Australia, or the American Cancer
Society. Given the strong association with these markers with breast cancer in
women, it is disappointing to discover that none of the societies even mention
these markers, and of course don't suggest that people track them.
Monitoring Cancer using the markers
Most of the markers
outlined above can be obtained with standard blood tests, hence the serum B12,
folate and Apoliprotein A
and B levels are standard tests. Persons who believe that may have cancer or who
have been treated for it can readily obtain this data and hence raise a
precautionary alarm to request further investigation, or follow the levels
following treatment to see if the rates rise.
Reference data
TBA
References
Kane et al. Vitamin B12 binding protein as a tumour marker for
hepatocellular carcinoma. Gut 1978 19:1105-9
Amado-Garzon
SB, Molina-Pimienta
L, Vejarano-Pombo
A, Vélez-Bonilla
M, Moreno-Chaparro
J, Buitrago-Lopez
A. Elevated Vitamin B12, Risk of Cancer, and Mortality: A Systematic Review.
Cancer Invest. 2024 Jul;42(6):515-526. doi:
10.1080/07357907.2024.2366907. Epub
2024 Jul 2. PMID:
38953509.
Liu K, Yang Z, Lu X, Zheng B, Wu S, Kang J, Sun S, Zhao J. The origin of vitamin
B12 levels and risk of all-cause, cardiovascular and cancer specific mortality:
A systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2024
Feb;117:105230. doi: 10.1016/j.archger.2023.105230. Epub 2023 Oct 11. PMID:
38252787.
Gimsing P, Hippe E. Increased concentration of transcobalamin I in a patient
with metastatic carcinoma of the breast. Scand J Haematol. 1978 Sep;21(3):243-9.
doi: 10.1111/j.1600-0609.1978.tb00359.x. PMID: 715376.
Sottotetti F, Malovini A, Maccarone S, Riva G, Tibollo V, Palumbo R, Tagliaferri
B, Bellazzi R, Cena H, Di Sabatino A, Locati LD, Lenti MV. Vitamin B12 status in
hospitalised cancer patients: Prevalence and clinical implications of depletion
and hypervitaminosis. Clin Nutr ESPEN. 2024 Oct;63:585-594. doi:
10.1016/j.clnesp.2024.07.017. Epub 2024 Jul 23. PMID: 39053694.
Collins DA, Hogenkamp HP, O'Connor MK, Naylor S, Benson LM, Hardyman TJ, Thorson
LM. Biodistribution of radiolabeled adenosylcobalamin in patients diagnosed with
various malignancies. Mayo Clin Proc. 2000 Jun;75(6):568-80. doi:
10.4065/75.6.568. PMID: 10852417.
Pirouzpanah S, Taleban FA, Mehdipour P, Atri M, Foroutan-Ghaznavi M. Plasma
total homocysteine level in association with folate, pyridoxine, and cobalamin
status among Iranian primary breast cancer patients. Nutr Cancer.
2014;66(7):1097-108. doi: 10.1080/01635581.2014.948213. Epub 2014 Aug 26. PMID:
25157842.
Collins etal Tumor imaging via Indium 111-labeled DTPA-adenosylcobalamin
Mayo Clin Proc. 1999 74:687-691
Kim JA,
Choi
R, Won H, Kim S,
Choi
HJ,
Ryu
JM,
Lee SK, Yu J, Kim SW, Lee JE,
Lee SY.
Serum Vitamin Levels and Their Relationships with Other Biomarkers in Korean
Breast Cancer Patients. Nutrients. 2020 Sep 16;12(9):2831. doi:
10.3390/nu12092831. PMID:
32947849; PMCID:
PMC7550996
Essén A, Santaolalla A, Garmo H, Hammar N, Walldius G, Jungner I, Malmström H,
Holmberg L, Van Hemelrijck M. Baseline serum folate, vitamin B12 and the risk of
prostate and breast cancer using data from the Swedish AMORIS cohort. Cancer
Causes Control. 2019 Jun;30(6):603-615. doi: 10.1007/s10552-019-01170-6. Epub
2019 Apr 24. PMID: 31020446.
Norman et al. Cobalamin (vitamin B12) deficiency detection by
urinary methylmalonic acid quantitation Blood 1982 59: 1128-31
Ermens, et al. Significance of elevated cobalamin (vitamin B12)
levels in blood.
PMID
14636871
Fanidi etal Is high vitamin B12 status a cause of lung cancer.
Int J Cancer 2019 146; 1499-1503
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6642017/
Russell-Jones, G.J 2022 Paradoxical B12 deficiency: Normal to elevated serum
vitamin B12 with metabolic vitamin B12 deficiency.
PDF
https://www.iomcworld.org/articles/paradoxical-vitamin-b12-deficiency-normal-to-elevated-serum-b12-with-metabolic-vitamin-b12-deficiency.pdf
Geissbühler, P., Mermillod, B., & Rapin, C. H. (2000). Elevated serum vitamin
B12 levels associated with CRP as a predictive factor of mortality in palliative
care cancer patients: a prospective study over five years. Journal of pain and
symptom management, 20(2), 93–103. https://doi.org/10.1016/s0885-3924(00)00169-x
Oh, H. K., Lee, J. Y., Eo, W. K., Yoon, S. W., & Han, S. N. (2018). Elevated
Serum Vitamin B12 Levels as a Prognostic Factor for Survival Time in Metastatic
Cancer Patients: A Retrospective Study. Nutrition and cancer, 70(1), 37–44.
https://doi.org/10.1080/01635581.2018.1397711
Aloreidi, K., & Zamulko, A. (2018). Elevated Vitamin B12: A Rare Presentation
for Gallbladder Adenocarcinoma. South Dakota medicine : the journal of the South
Dakota State Medical Association, 71(4), 171–173.
Lin, C. Y., Kuo, C. S., Lu, C. L., Wu, M. Y., & Huang, R. F. (2010). Elevated
serum vitamin B(12) levels in association with tumor markers as the prognostic
factors predictive for poor survival in patients with hepatocellular carcinoma.
Nutrition and cancer, 62(2), 190–197.
https://doi.org/10.1080/01635580903305334
Wakatsuki, Y., Inada, M., Kudo, H., Oshio, G., Masuda, T., Miyake, T., & Kita,
T. (1989). Immunological characterization and clinical implication of cobalamin
binding protein in human gastric cancer. Cancer research, 49(11), 3122–3128.
Lee, Y. Y., Wei, Y. C., Tian, Y. F., Sun, D. P., Sheu, M. J., Yang, C. C., Lin,
L. C., Lin, C. Y., Hsing, C. H., Li, W. S., Li, C. F., Hsieh, P. L., & Lin, C.
Y. (2017). Overexpression of Transcobalamin 1 is an Independent Negative
Prognosticator in Rectal Cancers Receiving Concurrent Chemoradiotherapy. Journal
of Cancer, 8(8), 1330–1337.
https://doi.org/10.7150/jca.18274<
Trehy, M. R., German, A. J., Silvestrini, P., Serrano, G., & Batchelor, D. J.
(2014). Hypercobalaminaemia is associated with hepatic and neoplastic disease in
cats: a cross sectional study. BMC
veterinary research, 10,
175.
https://doi.org/10.1186/s12917-014-0175-x
Waxman, S., Liu, C. K., Schreiber, C., & Helson, L. (1977). The clinical and
physiological implications of hepatoma B12-binding proteins. Cancer research,
37(6), 1908–1914.
Kane, S. P., Murray-Lyon, I. M., Paradinas, F. J., Johnson, P. J., Williams, R.,
Orr, A. H., & Kohn, J. (1978). Vitamin B12 binding protein as a tumour marker
for hepatocellular carcinoma. Gut, 19(12), 1105–1109.
https://doi.org/10.1136/gut.19.12.1105
Paradinas, F. J., Melia, W. M., Wilkinson, M. L., Portmann, B., Johnson, P. J.,
Murray-Lyon, I. M., & Williams, R. (1982). High serum vitamin B12 binding
capacity as a marker of the fibrolamellar variant of hepatocellular carcinoma.
British medical journal (Clinical research ed.), 285(6345), 840–842. https://doi.org/10.1136/bmj.285.6345.840
Carmel R. (1975). Extreme elevation of serum transcobalamin I in patients with
metastatic cancer. The New England journal of medicine, 292(6), 282–284.
https://doi.org/10.1056/NEJM197502062920603
Lacombe, V., Chabrun, F., Lacout, C. et
al. Persistent
elevation of plasma vitamin B12 is strongly associated with solid cancer. Sci
Rep 11, 13361
(2021). https://doi.org/10.1038/s41598-021-92945-y
Wolffenbuttel, B., Heiner-Fokkema, M. R., Green, R., & Gans, R. (2020).
Relationship between serum B12 concentrations and mortality: experience in
NHANES. BMC medicine, 18(1), 307.
https://doi.org/10.1186/s12916-020-01771-y
Arendt JF, Farkas DK,
Pedersen L, Nexo E, Sørensen HT. Elevated plasma vitamin B12 levels and cancer
prognosis: A population-based cohort study. (2016) Cancer epidemiology. 40:
158-65. doi:10.1016/j.canep.2015.12.007 - Pubmed
Haghighat G,
Khajeh-Mehrizi
A,
Ranjbar
H. Evaluation of Serum Vitamin B12 Levels in Patients with Colon and Breast
Cancer: A Case-Control Study. Int
J Hematol
Oncol
Stem Cell Res. 2023 Oct 1;17(4):240-244. doi:
10.18502/ijhoscr.v17i4.13914. PMID:
38076775; PMCID:
PMC10700096.
Matejcic M, de Batlle J, Ricci C, Biessy C, Perrier F, Huybrechts I, Weiderpass
E, Boutron-Ruault MC, Cadeau C, His M, Cox DG, Boeing H, Fortner RT, Kaaks R,
Lagiou P, Trichopoulou A, Benetou V, Tumino R, Panico S, Sieri S, Palli D,
Ricceri F, Bueno-de-Mesquita HB, Skeie G, Amiano P, Sánchez MJ, Chirlaque MD,
Barricarte A, Quirós JR, Buckland G, van Gils CH, Peeters PH, Key TJ, Riboli E,
Gylling B, Zeleniuch-Jacquotte A, Gunter MJ, Romieu I, Chajès V. Biomarkers of
folate and vitamin B12 and breast cancer risk: report from the EPIC cohort. Int
J Cancer. 2017 Mar 15;140(6):1246-1259. doi: 10.1002/ijc.30536. PMID: 27905104.
Arendt JF, Pedersen L,
Nexo E, Sørensen HT. Elevated plasma vitamin B12 levels as a marker for cancer:
a population-based cohort study. (2013) Journal of the National Cancer
Institute. 105 (23): 1799-805. doi:10.1093/jnci/djt315 - Pubmed
Russell-Jones G, McTavish K, McEwan J. Preliminary studies on the selective
accumulation of vitamin-targeted polymers within tumors. J Drug Target. 2011
Feb;19(2):133-9. doi: 10.3109/10611861003734027. Epub 2010 May 6. PMID:
20446757.
G.J.
Russell-Jones, K.
McTavish,
J.F.
McEwan,
in: Proceedings of the 2nd International Symposium on
Tumor
Targeted Delivery Systems, 2002
Russell-Jones G, McTavish K, McEwan J, Rice J, Nowotnik D. Vitamin-mediated
targeting as a potential mechanism to increase drug uptake by tumours. J Inorg
Biochem. 2004 Oct;98(10):1625-33. doi: 10.1016/j.jinorgbio.2004.07.009. PMID:
15458825. Paragomi P, Wang R, Huang JY, Midttun Ø, Ulvik A, Ueland PM, Koh
WP, Yuan JM, Luu HN. The Association Between Serum Riboflavin and Flavin
Mononucleotide With Pancreatic Cancer: Findings From a Prospective Cohort Study.
Pancreas. 2023 Feb 1;52(2):e127-e134. doi: 10.1097/MPA.0000000000002220. PMID:
37523604; PMCID: PMC10399971.
Long L, Pang XX, Zeng FM, Zhan XH, Xie YH, Pan F, Wang W, Liao LD, Xu XE, Li B,
Wang LD, Chang ZJ, Li EM, Xu LY. Promotion of rs3746804 (p. L267P) polymorphism
to intracellular SLC52A3a trafficking and riboflavin transportation in
esophageal cancer cells. Amino Acids. 2021 Aug;53(8):1197-1209. doi:
10.1007/s00726-021-03025-4. Epub 2021 Jul 5. PMID: 34223992.
Yu L, Tan Y, Zhu L. Dietary vitamin B2 intake and breast cancer risk: a
systematic review and meta-analysis. Arch Gynecol Obstet. 2017
Mar;295(3):721-729. doi: 10.1007/s00404-016-4278-4. Epub 2016 Dec 29. PMID:
28035488.
Ma Y, Huangfu Y, Deng L, Wang P, Shen L, Zhou Y. High serum riboflavin is
associated with the risk of sporadic colorectal cancer. Cancer Epidemiol. 2023
Apr;83:102342. doi: 10.1016/j.canep.2023.102342. Epub 2023 Feb 28. PMID:
36863217.
Xu L, Wu QX, Li X, Fang YJ, Zhou RL, Che MM, Ma T, Zhang CX. Serum flavin
mononucleotide but not riboflavin is inversely associated with the risk of
colorectal cancer. Food Funct. 2022 Nov 28;13(23):12246-12257. doi:
10.1039/d2fo02580a. PMID: 36342407.
Karande AA, Sridhar L, Gopinath KS, Adiga PR. Riboflavin carrier protein: a
serum and tissue marker for breast carcinoma. Int J Cancer. 2001 Sep
20;95(5):277-81. doi:
10.1002/1097-0215(20010920)95:5<277::aid-ijc1047>3.0.co;2-y. PMID: 11494224.
Darguzyte M, Holm R, Baier J, Drude N, Schultze J, Koynov K, Schwiertz D, Dadfar
SM, Lammers T, Barz M, Kiessling F. Influence of Riboflavin Targeting on Tumor
Accumulation and Internalization of Peptostar Based Drug Delivery Systems.
Bioconjug Chem. 2020 Dec 16;31(12):2691-2696. doi:
10.1021/acs.bioconjchem.0c00593. Epub 2020 Nov 25. PMID: 33237762.
Bartmann
L, Schumacher D, von
Stillfried
S,
Sternkopf
M, Alampour-Rajabi
S, van Zandvoort
MAMJ,
Kiessling
F, Wu Z. Evaluation of Riboflavin Transporters as Targets for Drug Delivery and
Theranostics.
Front Pharmacol.
2019 Feb 6;10:79. doi:
10.3389/fphar.2019.00079. Erratum in: Front
Pharmacol.
2020 Nov 26;11:617329. doi:
10.3389/fphar.2020.617329. Erratum in: Front
Pharmacol.
2022 Mar 31;13:894462. doi:
10.3389/fphar.2022.894462. PMID:
30787877; PMCID:
PMC6372557.
Yang HT,
Chao
PC, Yin MC. Riboflavin at high doses enhances lung cancer cell proliferation,
invasion, and migration. J Food
Sci.
2013 Feb;78(2):H343-9.
doi:
10.1111/1750-3841.12012. Epub
2013 Jan 11. PMID:
23311443
Ozsvari
B,
Bonuccelli
G, Sanchez-Alvarez R, Foster R,
Sotgia
F, Lisanti
MP. Targeting flavin-containing
enzymes eliminates cancer stem cells (CSCs),
by inhibiting mitochondrial respiration: Vitamin B2 (Riboflavin) in cancer
therapy. Aging (Albany NY). 2017 Dec 16;9(12):2610-2628.
doi:
10.18632/aging.101351. PMID:
29253841; PMCID:
PMC5764395.
Zhou Y,
Luo
G.
Apolipoproteins,
as the carrier proteins for lipids, are involved in the development of breast
cancer.
Clin
Transl
Oncol.
2020 Nov;22(11):1952-1962. doi:
10.1007/s12094-020-02354-2. Epub
2020 Apr 18. PMID:
32306242; PMCID:
PMC7505814.
Rao
PN,
Levine E, Myers MO,
Prakash
V, Watson J, Stolier
A, Kopicko
JJ,
Kissinger P, Raj
SG,
Raj
MH.
Elevation of serum riboflavin carrier protein in breast cancer. Cancer
Epidemiol
Biomarkers Prev.
1999 Nov;8(11):985-90. PMID:
10566553.
Rao
PN,
Crippin
J, Levine E, Hunt J, Baliga
S, Balart L, Anthony L, Mulekar
M, Raj
MH.
Elevation of serum riboflavin carrier protein in
hepatocellular
carcinoma. Hepatol
Res. 2006 Jun;35(2):83-7. doi:
10.1016/j.hepres.2006.03.009. Epub
2006 May 18. PMID:
16713333.
Bao
L,
Peng
J, Huang G, Wang S, Yin H, Wang T, Liu F, Sun G. [The study on the relationship
between serum folic acid and vitamin B2 levels and esophageal cancer].
Wei
Sheng
Yan
Jiu.
2013 May;42(3):451-4. Chinese. PMID:
23805525.
Several different types of cancers have been shown to have increased uptake of
folate (III-In-DTPA folate imaging)
Folate imaging has
been found to successfully detect metastatic cancers (Sega and Low 2008)
Many cancers have also been found to have
greatly increased uptake of biotin (Russell-Jones et al, 2002, 2004, 2008), with
many have dual uptake of vitamin B12 and biotin, or folate and biotin)
More recently, riboflavin has also been
found to target several tumours, and there are reports of elevated Riboflavin
Carrier Protein being associated with pancreatic cancer (Paragomi
et al, 2023). RIboflavin seems to play a dual role in cancers, in low riboflavin
there is an increased risk
of some cancers (Long et al, 2021; Yu et al, 2016), possibly due to its role in
maintaining the activity of MTHFR and MTRR and the methylation cycle. In a
similar fashion to the elevated serum B12 in some cancers, elevated serum
riboflavin has been seen in colorectal cancer (Ma et al, 2023; Xu et al, 2022),
Levels of the riboflavin carrier protein (RCP) are 3 to 4 times normal in many cases
of breast and other cancers (Karande et al, 2001;
Darguzyte
et al, 2020). Riboflavin uptake is greatly enhanced in some tumour cells (Bartmann
et al, 2019). Riboflavin supplementation has been shown to increase cancer cell
proliferation, invasion and migration, and inhibition of of flavin-containing
enzymes arrested tumor growth (Yang et al, 2013; Ozsvari et al, 2017).
Rao
and coworkers (1999) found that serum
RCP
levels were significantly elevated in women with breast cancer (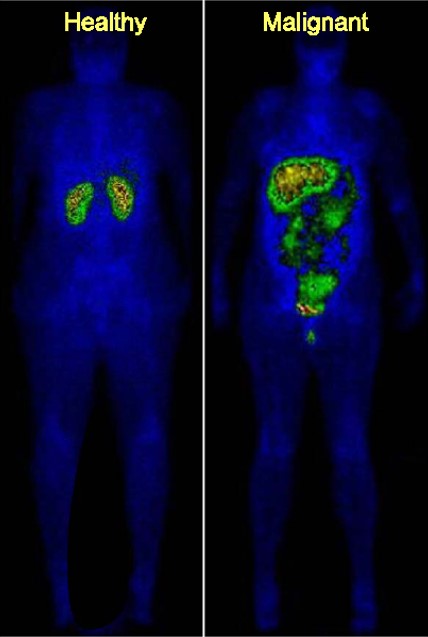
Biotin targeting to Cancers
Riboflavin targeting to Cancers
Riboflavin has also been shown to have an inhibitory role in some cancer, with levels of serum riboflavin lower in patients with esophageal cancer (Bao et al, 2013)
Measurement of Serum riboflavin, what does it mean?
In order to understand the data, and in order to stop the hysteria that may result from the concept that elevated riboflavin may be associated with cancer, one has to firstly understand what measurement of vitamin B2 in serum actually means.
Hence, Serum vitamin B2 is a measurement of circulating vitamin B2 that is either free, or is bound by a vitamin B2 binding protein. In the case of elevated serum vitamin B2, due to the presence of cancer, the cancer cells themselves have been shown to secrete a riboflavin binding protein, in an attempt to sequester vitamin B2 either from the diet, the liver or from supplementation. This the cancer will do, regardless of the amount of vitamin B2 supplemented or ingested. Logically, the lower the vitamin B2, the greater the expression of the vitamin B2 binding proteins. Since functional vitamin B2 deficiency can occur at any serum level, so too can "relatively" elevated vitamin B2. Hence the measurement of serum vitamin B2 should be done in comparison to levels before or after identification or treatment of cancer.
Associated Factors - Apolipoproteins
Elevations in Apoliproteins have been found to be associated with several cancers. ApoB, and ApoA have been shown to have potential as diagnostic markers (Zhou and Luo, 2020)
Ferritin
Ferritin is differentially over-expressed in tissues from multiple malignancies,
including: hepatocellular carcinoma [46], [47], Hodgkin's lymphoma [48], breast
cancer [49], [50], [51], [52], [53], and pancreatic cancer [50]
Relevance of the elevated serum markers
There is strong evidence to suggest that the treatment of various cancers could be followed by monitoring the serum markers. Potentially they could be used in the initial diagnosis. There is some debated about what to do, if you find the elevated markers, whether to supplement or not. Evidence suggests that the reason for the elevated markers was some sort of nutritional deficiency in the first. This then resulted in lower methylation and thereby poorer control of oncogene expression. Unfortunately, very, very clinicians know of the associations not do National Cancer bodies such as the Cancer Council of Australia, or the American Cancer Society. Given the strong association with these markers with breast cancer in women, it is disappointing to discover that none of the societies even mention these markers, and of course don't suggest that people track them.
Monitoring Cancer using the markers
Most of the markers outlined above can be obtained with standard blood tests, hence the serum B12, folate and Apoliprotein A and B levels are standard tests. Persons who believe that may have cancer or who have been treated for it can readily obtain this data and hence raise a precautionary alarm to request further investigation, or follow the levels following treatment to see if the rates rise.
Reference data
TBA
References
Kane et al. Vitamin B12 binding protein as a tumour marker for hepatocellular carcinoma. Gut 1978 19:1105-9
Amado-Garzon SB, Molina-Pimienta L, Vejarano-Pombo A, Vélez-Bonilla M, Moreno-Chaparro J, Buitrago-Lopez A. Elevated Vitamin B12, Risk of Cancer, and Mortality: A Systematic Review. Cancer Invest. 2024 Jul;42(6):515-526. doi: 10.1080/07357907.2024.2366907. Epub 2024 Jul 2. PMID: 38953509.
Liu K, Yang Z, Lu X, Zheng B, Wu S, Kang J, Sun S, Zhao J. The origin of vitamin B12 levels and risk of all-cause, cardiovascular and cancer specific mortality: A systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2024 Feb;117:105230. doi: 10.1016/j.archger.2023.105230. Epub 2023 Oct 11. PMID: 38252787.
Gimsing P, Hippe E. Increased concentration of transcobalamin I in a patient with metastatic carcinoma of the breast. Scand J Haematol. 1978 Sep;21(3):243-9. doi: 10.1111/j.1600-0609.1978.tb00359.x. PMID: 715376.
Sottotetti F, Malovini A, Maccarone S, Riva G, Tibollo V, Palumbo R, Tagliaferri B, Bellazzi R, Cena H, Di Sabatino A, Locati LD, Lenti MV. Vitamin B12 status in hospitalised cancer patients: Prevalence and clinical implications of depletion and hypervitaminosis. Clin Nutr ESPEN. 2024 Oct;63:585-594. doi: 10.1016/j.clnesp.2024.07.017. Epub 2024 Jul 23. PMID: 39053694.
Collins DA, Hogenkamp HP, O'Connor MK, Naylor S, Benson LM, Hardyman TJ, Thorson LM. Biodistribution of radiolabeled adenosylcobalamin in patients diagnosed with various malignancies. Mayo Clin Proc. 2000 Jun;75(6):568-80. doi: 10.4065/75.6.568. PMID: 10852417.
Pirouzpanah S, Taleban FA, Mehdipour P, Atri M, Foroutan-Ghaznavi M. Plasma total homocysteine level in association with folate, pyridoxine, and cobalamin status among Iranian primary breast cancer patients. Nutr Cancer. 2014;66(7):1097-108. doi: 10.1080/01635581.2014.948213. Epub 2014 Aug 26. PMID: 25157842.
Collins etal Tumor imaging via Indium 111-labeled DTPA-adenosylcobalamin Mayo Clin Proc. 1999 74:687-691
Kim JA, Choi R, Won H, Kim S, Choi HJ, Ryu JM, Lee SK, Yu J, Kim SW, Lee JE, Lee SY. Serum Vitamin Levels and Their Relationships with Other Biomarkers in Korean Breast Cancer Patients. Nutrients. 2020 Sep 16;12(9):2831. doi: 10.3390/nu12092831. PMID: 32947849; PMCID: PMC7550996
Essén A, Santaolalla A, Garmo H, Hammar N, Walldius G, Jungner I, Malmström H, Holmberg L, Van Hemelrijck M. Baseline serum folate, vitamin B12 and the risk of prostate and breast cancer using data from the Swedish AMORIS cohort. Cancer Causes Control. 2019 Jun;30(6):603-615. doi: 10.1007/s10552-019-01170-6. Epub 2019 Apr 24. PMID: 31020446.
Norman et al. Cobalamin (vitamin B12) deficiency detection by urinary methylmalonic acid quantitation Blood 1982 59: 1128-31
Ermens, et al. Significance of elevated cobalamin (vitamin B12) levels in blood. PMID 14636871
Fanidi etal Is high vitamin B12 status a cause of lung cancer. Int J Cancer 2019 146; 1499-1503 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6642017/
Russell-Jones, G.J 2022 Paradoxical B12 deficiency: Normal to elevated serum vitamin B12 with metabolic vitamin B12 deficiency. PDF https://www.iomcworld.org/articles/paradoxical-vitamin-b12-deficiency-normal-to-elevated-serum-b12-with-metabolic-vitamin-b12-deficiency.pdf
Geissbühler, P., Mermillod, B., & Rapin, C. H. (2000). Elevated serum vitamin
B12 levels associated with CRP as a predictive factor of mortality in palliative
care cancer patients: a prospective study over five years. Journal of pain and
symptom management, 20(2), 93–103. https://doi.org/10.1016/s0885-3924(00)00169-x
Oh, H. K., Lee, J. Y., Eo, W. K., Yoon, S. W., & Han, S. N. (2018). Elevated
Serum Vitamin B12 Levels as a Prognostic Factor for Survival Time in Metastatic
Cancer Patients: A Retrospective Study. Nutrition and cancer, 70(1), 37–44.
https://doi.org/10.1080/01635581.2018.1397711
Aloreidi, K., & Zamulko, A. (2018). Elevated Vitamin B12: A Rare Presentation for Gallbladder Adenocarcinoma. South Dakota medicine : the journal of the South Dakota State Medical Association, 71(4), 171–173.
Lin, C. Y., Kuo, C. S., Lu, C. L., Wu, M. Y., & Huang, R. F. (2010). Elevated serum vitamin B(12) levels in association with tumor markers as the prognostic factors predictive for poor survival in patients with hepatocellular carcinoma. Nutrition and cancer, 62(2), 190–197. https://doi.org/10.1080/01635580903305334
Wakatsuki, Y., Inada, M., Kudo, H., Oshio, G., Masuda, T., Miyake, T., & Kita, T. (1989). Immunological characterization and clinical implication of cobalamin binding protein in human gastric cancer. Cancer research, 49(11), 3122–3128.
Lee, Y. Y., Wei, Y. C., Tian, Y. F., Sun, D. P., Sheu, M. J., Yang, C. C., Lin, L. C., Lin, C. Y., Hsing, C. H., Li, W. S., Li, C. F., Hsieh, P. L., & Lin, C. Y. (2017). Overexpression of Transcobalamin 1 is an Independent Negative Prognosticator in Rectal Cancers Receiving Concurrent Chemoradiotherapy. Journal of Cancer, 8(8), 1330–1337. https://doi.org/10.7150/jca.18274<
Trehy, M. R., German, A. J., Silvestrini, P., Serrano, G., & Batchelor, D. J. (2014). Hypercobalaminaemia is associated with hepatic and neoplastic disease in cats: a cross sectional study. BMC veterinary research, 10, 175. https://doi.org/10.1186/s12917-014-0175-x
Waxman, S., Liu, C. K., Schreiber, C., & Helson, L. (1977). The clinical and physiological implications of hepatoma B12-binding proteins. Cancer research, 37(6), 1908–1914.
Kane, S. P., Murray-Lyon, I. M., Paradinas, F. J., Johnson, P. J., Williams, R., Orr, A. H., & Kohn, J. (1978). Vitamin B12 binding protein as a tumour marker for hepatocellular carcinoma. Gut, 19(12), 1105–1109. https://doi.org/10.1136/gut.19.12.1105
Paradinas, F. J., Melia, W. M., Wilkinson, M. L., Portmann, B., Johnson, P. J., Murray-Lyon, I. M., & Williams, R. (1982). High serum vitamin B12 binding capacity as a marker of the fibrolamellar variant of hepatocellular carcinoma. British medical journal (Clinical research ed.), 285(6345), 840–842. https://doi.org/10.1136/bmj.285.6345.840
Carmel R. (1975). Extreme elevation of serum transcobalamin I in patients with metastatic cancer. The New England journal of medicine, 292(6), 282–284. https://doi.org/10.1056/NEJM197502062920603
Lacombe, V., Chabrun, F., Lacout, C. et al. Persistent elevation of plasma vitamin B12 is strongly associated with solid cancer. Sci Rep 11, 13361 (2021). https://doi.org/10.1038/s41598-021-92945-y
Wolffenbuttel, B., Heiner-Fokkema, M. R., Green, R., & Gans, R. (2020). Relationship between serum B12 concentrations and mortality: experience in NHANES. BMC medicine, 18(1), 307. https://doi.org/10.1186/s12916-020-01771-y
Arendt JF, Farkas DK, Pedersen L, Nexo E, Sørensen HT. Elevated plasma vitamin B12 levels and cancer prognosis: A population-based cohort study. (2016) Cancer epidemiology. 40: 158-65. doi:10.1016/j.canep.2015.12.007 - Pubmed
Haghighat G, Khajeh-Mehrizi A, Ranjbar H. Evaluation of Serum Vitamin B12 Levels in Patients with Colon and Breast Cancer: A Case-Control Study. Int J Hematol Oncol Stem Cell Res. 2023 Oct 1;17(4):240-244. doi: 10.18502/ijhoscr.v17i4.13914. PMID: 38076775; PMCID: PMC10700096.Matejcic M, de Batlle J, Ricci C, Biessy C, Perrier F, Huybrechts I, Weiderpass E, Boutron-Ruault MC, Cadeau C, His M, Cox DG, Boeing H, Fortner RT, Kaaks R, Lagiou P, Trichopoulou A, Benetou V, Tumino R, Panico S, Sieri S, Palli D, Ricceri F, Bueno-de-Mesquita HB, Skeie G, Amiano P, Sánchez MJ, Chirlaque MD, Barricarte A, Quirós JR, Buckland G, van Gils CH, Peeters PH, Key TJ, Riboli E, Gylling B, Zeleniuch-Jacquotte A, Gunter MJ, Romieu I, Chajès V. Biomarkers of folate and vitamin B12 and breast cancer risk: report from the EPIC cohort. Int J Cancer. 2017 Mar 15;140(6):1246-1259. doi: 10.1002/ijc.30536. PMID: 27905104.
Arendt JF, Pedersen L, Nexo E, Sørensen HT. Elevated plasma vitamin B12 levels as a marker for cancer: a population-based cohort study. (2013) Journal of the National Cancer Institute. 105 (23): 1799-805. doi:10.1093/jnci/djt315 - Pubmed
Russell-Jones G, McTavish K, McEwan J. Preliminary studies on the selective accumulation of vitamin-targeted polymers within tumors. J Drug Target. 2011 Feb;19(2):133-9. doi: 10.3109/10611861003734027. Epub 2010 May 6. PMID: 20446757.
G.J. Russell-Jones, K. McTavish, J.F. McEwan, in: Proceedings of the 2nd International Symposium on Tumor Targeted Delivery Systems, 2002
Russell-Jones G, McTavish K, McEwan J, Rice J, Nowotnik D. Vitamin-mediated targeting as a potential mechanism to increase drug uptake by tumours. J Inorg Biochem. 2004 Oct;98(10):1625-33. doi: 10.1016/j.jinorgbio.2004.07.009. PMID: 15458825. Paragomi P, Wang R, Huang JY, Midttun Ø, Ulvik A, Ueland PM, Koh WP, Yuan JM, Luu HN. The Association Between Serum Riboflavin and Flavin Mononucleotide With Pancreatic Cancer: Findings From a Prospective Cohort Study. Pancreas. 2023 Feb 1;52(2):e127-e134. doi: 10.1097/MPA.0000000000002220. PMID: 37523604; PMCID: PMC10399971.
Long L, Pang XX, Zeng FM, Zhan XH, Xie YH, Pan F, Wang W, Liao LD, Xu XE, Li B, Wang LD, Chang ZJ, Li EM, Xu LY. Promotion of rs3746804 (p. L267P) polymorphism to intracellular SLC52A3a trafficking and riboflavin transportation in esophageal cancer cells. Amino Acids. 2021 Aug;53(8):1197-1209. doi: 10.1007/s00726-021-03025-4. Epub 2021 Jul 5. PMID: 34223992.
Yu L, Tan Y, Zhu L. Dietary vitamin B2 intake and breast cancer risk: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017 Mar;295(3):721-729. doi: 10.1007/s00404-016-4278-4. Epub 2016 Dec 29. PMID: 28035488.
Ma Y, Huangfu Y, Deng L, Wang P, Shen L, Zhou Y. High serum riboflavin is associated with the risk of sporadic colorectal cancer. Cancer Epidemiol. 2023 Apr;83:102342. doi: 10.1016/j.canep.2023.102342. Epub 2023 Feb 28. PMID: 36863217.
Xu L, Wu QX, Li X, Fang YJ, Zhou RL, Che MM, Ma T, Zhang CX. Serum flavin mononucleotide but not riboflavin is inversely associated with the risk of colorectal cancer. Food Funct. 2022 Nov 28;13(23):12246-12257. doi: 10.1039/d2fo02580a. PMID: 36342407.
Karande AA, Sridhar L, Gopinath KS, Adiga PR. Riboflavin carrier protein: a serum and tissue marker for breast carcinoma. Int J Cancer. 2001 Sep 20;95(5):277-81. doi: 10.1002/1097-0215(20010920)95:5<277::aid-ijc1047>3.0.co;2-y. PMID: 11494224.
Darguzyte M, Holm R, Baier J, Drude N, Schultze J, Koynov K, Schwiertz D, Dadfar SM, Lammers T, Barz M, Kiessling F. Influence of Riboflavin Targeting on Tumor Accumulation and Internalization of Peptostar Based Drug Delivery Systems. Bioconjug Chem. 2020 Dec 16;31(12):2691-2696. doi: 10.1021/acs.bioconjchem.0c00593. Epub 2020 Nov 25. PMID: 33237762.
Bartmann L, Schumacher D, von Stillfried S, Sternkopf M, Alampour-Rajabi S, van Zandvoort MAMJ, Kiessling F, Wu Z. Evaluation of Riboflavin Transporters as Targets for Drug Delivery and Theranostics. Front Pharmacol. 2019 Feb 6;10:79. doi: 10.3389/fphar.2019.00079. Erratum in: Front Pharmacol. 2020 Nov 26;11:617329. doi: 10.3389/fphar.2020.617329. Erratum in: Front Pharmacol. 2022 Mar 31;13:894462. doi: 10.3389/fphar.2022.894462. PMID: 30787877; PMCID: PMC6372557.
Yang HT, Chao PC, Yin MC. Riboflavin at high doses enhances lung cancer cell proliferation, invasion, and migration. J Food Sci. 2013 Feb;78(2):H343-9. doi: 10.1111/1750-3841.12012. Epub 2013 Jan 11. PMID: 23311443
Ozsvari B, Bonuccelli G, Sanchez-Alvarez R, Foster R, Sotgia F, Lisanti MP. Targeting flavin-containing enzymes eliminates cancer stem cells (CSCs), by inhibiting mitochondrial respiration: Vitamin B2 (Riboflavin) in cancer therapy. Aging (Albany NY). 2017 Dec 16;9(12):2610-2628. doi: 10.18632/aging.101351. PMID: 29253841; PMCID: PMC5764395.
Zhou Y, Luo G. Apolipoproteins, as the carrier proteins for lipids, are involved in the development of breast cancer. Clin Transl Oncol. 2020 Nov;22(11):1952-1962. doi: 10.1007/s12094-020-02354-2. Epub 2020 Apr 18. PMID: 32306242; PMCID: PMC7505814.
Rao PN, Levine E, Myers MO, Prakash V, Watson J, Stolier A, Kopicko JJ, Kissinger P, Raj SG, Raj MH. Elevation of serum riboflavin carrier protein in breast cancer. Cancer Epidemiol Biomarkers Prev. 1999 Nov;8(11):985-90. PMID: 10566553.
Rao PN, Crippin J, Levine E, Hunt J, Baliga S, Balart L, Anthony L, Mulekar M, Raj MH. Elevation of serum riboflavin carrier protein in hepatocellular carcinoma. Hepatol Res. 2006 Jun;35(2):83-7. doi: 10.1016/j.hepres.2006.03.009. Epub 2006 May 18. PMID: 16713333.
Bao
L,
Peng
J, Huang G, Wang S, Yin H, Wang T, Liu F, Sun G. [The study on the relationship
between serum folic acid and vitamin B2 levels and esophageal cancer].
Wei
Sheng
Yan
Jiu.
2013 May;42(3):451-4. Chinese. PMID:
23805525.
Copyright © 2018 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited