
Vitamin B12 Deficiency and COVID
-
COVID-19 is a coronavirus, which is potentially lethal, especially in the elderly
-
Predisposing factors are age, high blood pressure, heart disease, and diabetes, and in around 90% of deaths, there was at least one co-morbidity.
-
Resistance to COVID-19 morbidity appears to drop as production of melatonin decreases with age
-
Factors affecting production of melatonin, such as vitamin B12 levels, and the levels of supporting vitamins and minerals will therefore affect resistance to COVID-19 sequelae
-
Resistance to COVID-19 in China has been found to be proportional to regional Selenium concentrations
-
Survivors of COVID-19 infection can develop Long COVID, the severity of which is dependent upon the reduced levels of factors, which would normally convey resistance to the virus.
-
Paradoxical B12 deficiency is associated with a higher risk of admission to ICU, the need for ventilators and death from COVID-19
COVID-19 Infection
-
The COVID-19 virus enters cells via ACE-2 receptors on cells
-
Expression of ACE-2 receptors is increased with the use of ACE-2 receptor blockers (ARBs)
-
Potentially the use of the ARBs could increase the uptake of COVID-19
-
This may explain why people on anti-hypertensive medication are more at risk of COVID-19 infections.
-
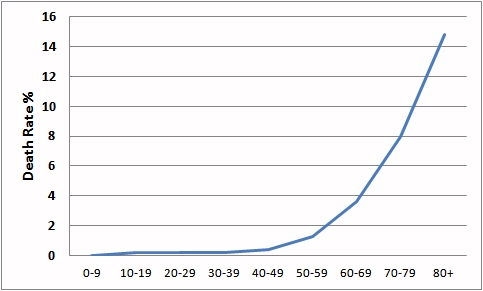
Risk factors for COVID-19 related deaths include increased signs of sepsis, high blood pressure, heart disease CVD increase 10.6%, lung disease 7.3%, diabetes 6.3%, being immuno-suppressed 5.6% and blood clotting issues, however, the greatest risk is with increasing age.
-
In some regards, the death rate is more dependent upon the standard of health care than any thing else with death rates of only 1-2% in countries such as Israel and Australia, but as high as 11.8, 19 and 11.8% in Spain, France and Italy respectively (as of 26/03/20). This is going to be catastrophic in Africa, where death rates from the flu are very high.
Potential increase in Infection with ACE inhibitors
Many of the anti-hypertensive medicines, including Captopril and
enalapril, and also selenopril directly interact with ACE and inhibit their
action. Potentially, though, the reduce activity of ACE would lead to an
up-regulation of ACE by the cells, and hence provide more receptors for COVID-19
to bind to, thereby increasing the severity of the infection. Recently a new
inhibitor selenoneine has been identified as a potential ACE inhibitor (Seko
etal, 2019). Whilst this molecule, a selenium-containing imidazole, does contain
Selenium, its action is completely different to that of dietary or supplemental
Selenite, which is involved in production of Selenoproteins.
Melatonin, together with vitamin D, stimulates neuronal stem
cells to differentiate into oligodendrocytes, which are the cells in the brain
that are responsible for myelination of the nerves in the brain. Melatonin is
thus critically important in the young for neuronal development as the child
grows and matures. Production of melatonin gradually starts to
decline after puberty. To date there have been no fatalities due to COVID-19 in
children under the age of 9, and there is a gradual increase in fatality rate
with age, which is inversely proportional to the drop in melatonin
production with age (Gravid etal, 2007). One reason postulated for this is
melatonin's unique ability to inhibit the activation of the inflammatory
cascade. In this way destruction of mitochondrial energy production during the
inflammatory response can be inhibited. In the lung, the site of COVID-19
infection, melatonin can thereby inhibit the acute respiratory distress
syndrome, thereby reducing the damage to the lungs and thereby the need for
intubation and mechanical ventilation of the lungs, with the associated damage
(Wu etal, 2020). Melatonin has also been shown to be protective against multiple
organ failure, circulatory failure, as well as preventing mitochondrial damage
in experimental sepsis, and able to reduce lipid peroxidation, one of the
indices of inflammation and mortality in human newborns with sepsis (Escames
etal, 2006; Lopez etal 2006; Escames etal, 2005; Carillo-Vico etal, 2005;
Srinivasan etal, 2010; Reiter etal, 2001; 2017; Biancatelli etal 2020) Melatonin
has also been shown to modulate the inflammatory response through its modulation
of Inflammasome activation (Favero etal, 2017)
Melatonin levels as we aget
Grivas and Savvidou, 2007
COVID-19 fatality rate by age (China)
Production of melatonin is critically dependent upon maintaining sufficient
levels of the methylating agent, S-Adenosylmethionine, a product of the
methylation cycle, a cycle which is dependent on functional activity of methyl
vitamin B12. Functional activity of vitamin B12 is in turn dependent upon
functional vitamin B2, or more specifically FMN and FAD. Production of FMN and
FAD, is in turn is dependent upon intake of vitamin B2, Iodine, Selenium and
Molybdenum. Deficiencies in any or all of these will lead to lower active
vitamin B2 being present, and from there lower active methyl B12, and hence
lower levels of melatonin. Potentially there is another reason for higher
lethality in those with low melatonin, and that is the potential accumulation of
the adrenalin pre-cursor- serotonin, leading to serotonin levels typically seen
in serotonin syndrome, a syndrome that has been associated with acute pulmonary edema (Wu etal, 2015; Shah and Jain, 2016; Ferslew etal, 1998). Vitamin B12 has
long been known to have a role in damping down the inflammatory response via
several mechanisms Scavenging of
Nitric Oxide Inhibition of
NFkappaB, an important inflammatory mediator More recently
high dose intravenous Methyl B12 has been suggested as a safe and cost
effective treatment for the Acute Respiratory Distress Syndrome, that is one
of the major causes of death from COVID-19 (Wheatley, 2006; Manzanares and
Hardy, 2010). If this is found to be true, then
one would assume that daily topical administration of Methyl B12 in Transdermoil
Vitamin B12
and the Production of Melatonin

Vitamin B12
and the inflammatory Response
Selenium and the inflammatory Response
High dose sodium selenite given to patients with severe systemic inflammatory response syndrome, sepsis, and septic shock, was found to reduce mortality rate (Angstwurm etal, 2007). The virulence of several respiratory viruses was found to be increased in Selenium deficient mice (Beck etal, 2003; 2001; 1994). Selenium supplementation with 200 ug/day selenium has been found to reduce the viral load in HIV (Hurwitz etal, 2007; Baum etal, 1997). Recent data analysis from China has shown that the areas with the highest Selenium concentrations has lower death rates than those with low Selenium. Selenium potentially has many roles in protection. It is required as a cofactor by glutathione peroxidase, which is involved in inactivating inflammatory hydrogen peroxide. It is critical in the activation of vitamin B2, and in thereby in maintaining free glutathione inside the cells, and active B2 (as FMN and FAD) are both required to maintain the activity of methylB12, and so is involved in the production of melatonin. Levels of Selenium decline in the body with age, and are generally lower in males, due to the targeting of Selenium to the testes, hence potentially explaining the higher death rate in males than females of the same age.
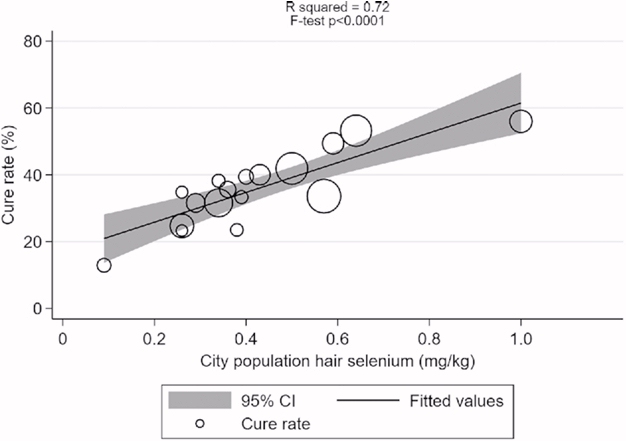
Zhang etal, 2020
Resistance to COVID-19 in China has been reported to be correlated with regional Selenium status (Zhang etal, 2020, Rayman etal, 2020).
Part of the inflammatory cascade involves the activation of oxygen by NADPH Oxidase to generate the reactive oxygen species O2**, This in turn is further activated to generate hydrogen peroxide (H2O2). Under normal circumstances the H2O2 is then converted to hydroxide and then water by the Selenoprotein Glutathione-Peroxidase (GSHPx(Se).
In Selenium deficiency this reaction is reduced and so dangerous H2O2 would accumulate inside the cell and cause massive intracellular damage. Further, the reduction of oxidized glutathione (GSSG) requires the FAD-dependent enzyme glutathione reductase (GSH reductase). In Selenium deficiency activation of vitamin B2 is incomplete and hence levels of FMN and FAD would be lower inside the cell. This has the dual effect of reducing the activity of GSH-reductase, but also, because of the requirement for FMN and FAD in the cycling of methyl B12, lack of FMN and FAD would lead to lower methylation and reduced production of GSH, through lower activity of the sulphation cycle in Methyl B12 deficiency. The result would be a greatly increased reaction of H2O2 and potentially cause death due to an over-active inflammatory response - Inflammatory storm.
Studies in which glutathione production has been inhibited have shown to result in very high levels of free radicals accumulating within cells (Kurniawan etal, 2020), further supporting the hypothesis that reduced GSHPx and GSH reductase activity can result in massively increased oxygen radical damage. Uncontrolled NADPH-oxidase have been shown to play a critical role in Hyperoxia-induced acute lung injury (Carnesecchi etal 2009). Hyperoxia has also been shown to increase ROS production by human pulmonary artery endothelial cells (Parinandi etal, 2003). NADPH oxidase activity in inflammasomes has also been shown to be responsible for the production of pulmonary fibrosis, a feature of COVID-19 infections (Sun etal, 2015). Potentially hyperoxygenation of the lungs during Ventilator treatment could potentiate the ROS damage, particularly in those that are Selenium, or B12 deficient (Carnesecchi eta. This may explain the very high death rate (92%) in those over 65 who are placed on ventilators. Despite these associations, no Health expert has yet to suggest that populations supplement with Selenium. As of 13/05/2020, there were 286,000 deaths from COVID-19. How many of these could have been prevented just by adequate Selenium supplementation?
Iron and Resistance to Respiratory infections
Iron deficiency has been associated with an increased susceptibility to respiratory infections (Jayaweera etal, 2019; Stepan etal, 2018; Tansarli etal 2013), and with a poorer outcome in patients with other respiratory infections, such as influenza A (H1N1)(Bai etal, 2010;. Iron deficiency has also been associated with a poorer outcome for congestive heart failure, a potential complication of Coronavirus infection (Nickol etal, 2015). Iron supplementation has been shown to reduce morbidity due to upper respiratory infections (de Silva etal, 2003; Hurrell 2007). Persons using PPIs for treatment of obesity are known to have lower iron levels (Yu etal, 2017), and as such might be expected to have higher incidence of URTI. Iron is also essential for energy production and for carrying oxygen, hence a deficiency of iron could contribute to respiratory failure seen in COVID patients.
Zinc and Resistance to Respiratory infections
Along with iron, zinc deficiency has been associated with an increased incidence of acute respiratory infections (Bailey etal, 2015)
Vitamin B12 Deficiency and Energy metabolism
Vitamin B12 has a critical role in energy production through it's role in production of CoQ10, creatine, and its role in the production of the Krebs cycle enzyme, aconitase. Hence decreased levels of active B12 should be correlated with lower metabolic energy in Krebs may be associated with reduced energy production and as such may contribute to respiratory failure in COVID-19 patients.
Death from COVID-19 and Paradoxical B12 Deficiency
Recent studies have shown that the probability of admission to ICU, of Intubation and death, rose the higher the Paradoxical B12 deficiency (Ersoz and Yulmiz 2021; Galmes et al,2020; Dalbeni et al. 2021). In addition COVID deaths are associated with elevated homocysteine, and lower creatinine (Galmes et al, 2020)
:
Serum Vitamin B12 in COVID-patients (Dalbeni etal, 2021)

Serum vitamin B12 vs COVID deaths
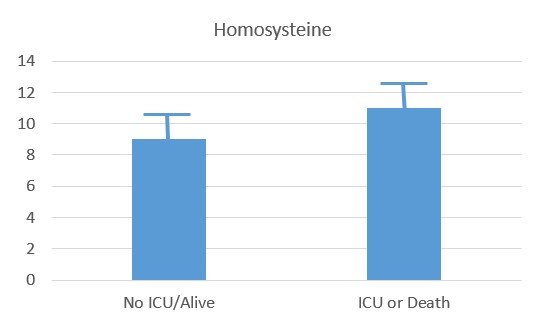
Serum Homocysteine in COVID-patients (Dalbeni et al, 2021)
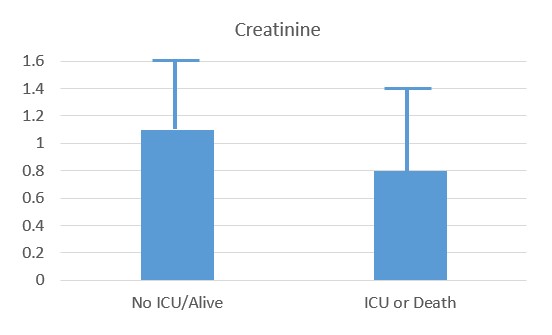
Reduced creatinine associated with ICU and Death
Vitamin D Deficiency and Respiratory Infections
Studies have reported a consistent association between low serum concentrations of 25-OH-Vitamin D and susceptibility to acute respiratory tract infections (Martinez etal, 2017; Ginde etal, 2009; Joliffe etal, 2013: Kim etal, 2015; Remmelts etal, 2012; Leow etal, 2011; Mathias etal 2015). Vitamin D supplementation has also been shown to reduce mortality to respiratory tract infections, particularly in the elderly (Bjelakovic etal, 2011). Current suggestions are supplementation with 1000-4000 IU of vitamin D per day, with bolus supplementation (ie once per week) not recommended (Sizar etal 2020). It has been suggested that the heavy mortality observed following Coronavius infection may be associated with low vitamin D levels in countries such as Italy, and Scandinavia. Low vitamin D is also prevalent in the UK, with a rise in rickets being seen in children. Vitamin D has been shown to decrease the production of pro-inflammatory molecules, and as such may reduce the "cytokine storm" that is associated with the pathogenesis of COVID-19. Vitamin D has also been shown to be essential for immune function, and low vitamin D is associated with greater susceptibility to both bacterial and viral infections. Vitamin D levels tend to decrease with age, as too vitamin D deficiency associated conditions such as diabetes and obesity, all three of which have been associated with mortality to COVID-19. In Ireland, 47% of people over 85 are deficient in vitamin D, with 27% of those over 70. Vitamin D deficiency is very common in the community with 42% of Americans deemed vitamin D deficient. Deficiency increases in black people (82%) and Hispanics (70%). The highest death rate in the US occurs in African-Americans. In nursing homes in Australia, where a significant number of cases of deaths, 86% of women, and 68% of men were found to have vitamin levels below 28 nmols/litre. Despite the known protective effect of vitamin D, no health authority has yet to suggest that the population increase their vitamin D. This alone could halve the death rate from COVID-19 and also reduce the deaths from seasonal flu. Studies have now shown that despite the success of the smart sun campaigns, such as the slip, slop, slap campaign, which is largely responsible for the lowering of the population vitamin D levels, there has been little change in the incidence of melanoma. Many studies have now shown that the severity of COVID-19 infections is greatly increased in those with low vitamin D (Weir etal, 2020; De Smet etal, 2021; Xu etal, 2020; Pizzini etal, 2020; Ali, 2020; Basaran, etal, 2021). Despite this no health authority has suggested that persons maximize vitamin D levels to protect themselves against the severity of COVID, and to reduce the mortality from COVID-19.
Death Rates from COVID-19
Death rates from COVID-19 vary greatly from country to country, with some recording death rates from infection as low as 0.4%, but others with death rates as high as 12%. Thus, whilst within a country the predisposing factors are high blood pressure, heart disease CVD ^ 10.6%, lung disease ^ 7.3%, diabetes ^ 6.3%, being immunosuppressed ^ 5.6% and blood clotting issues, and age, by far the biggest predisposing factor for the death is the country in which you live, which depending upon country can vary from a death rate of less than 0.6% to over 12%. Currently it is unknown why the rates vary, however, if these reasons could be identified it may go a long way to reducing the severity of the condition, which will be an essential component of dealing with the virus, particularly during the waiting period between now and the development of a vaccine. This will be more even more important if a successful vaccine is not developed. We have dedicated a separate page to a discussion of possible causes of the varying death rates..
Nutritional Support for Dealing with COVID-19
Vitamin A. Vitamin A was originally thought of as the anti-infective vitamin, and vitamin A deficiency has been implicated in the severity of diarrhoea and measles. Supplementation with vitamin A has reduced the morbidity and severity of a range of infectious diseases including HIV, malaria, measles and measles-related pneumonia (Semba 1999). The ability to generate an immune response to inactivated bovine coronavirus vaccines is compromised in calves with low vitamin A (Lee etal, 2013).
Vitamin C. Vitamin C has been shown to support immune function and to be able to protect against coronavirus infections (Hemila 2003). Vitamin C is also essential for the formation of hydroxyproline, an essential amino acid for the production of high tensile collagen. Lack of vitamin C, could potentially lead to alveolar collapse, due to "weak" collagen.
Vitamin D. Vitamin D has known immune functions including stimulation of maturation of immune cells, but also in activation of several proteins in Krebs cycle. Decreased vitamin D levels in calves has been reported to increase susceptibility of calves to bovine Coranavirus (Nonnecke etal, 2014). Potentially the greatly reduced vitamin D levels in the population due to the adoption of high SPF cosmetics, could increase the morbidity and mortality to coronavirus. Activation of vitamin D requires adequate amounts of iron, activated vitamin B2 (FAD), vitamin B12 and folate. Interestingly, vitamin D levels were very low in Italy, one of the countries with the highest death rate from COVID-19 (Giustina etal, 2020; Garami 2020). Potentially doubling the vitamin D levels in the population could have a much more beneficial effect than any of the molecules currently under study to aid in reducing the inflammatory storm. Trials with high dose vitamin D in those infected with COVID-19 showed quicker resolution of the infection. (Rastogi etal, 2020)
Selenium. Selenium has an important role in the body, not only in anti-oxidant defense but also in the activation of vitamin B2, and then the activation of vitamin B6, vitamin K and also for vitamin A. High dose sodium selenite has been found to reduce viral loads, and to reduce mortality in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Selenium is also a vital mineral for the activation of vitamin B2 .
Vitamin B2. Activation of vitamin B12, vitamin B6, vitamin A and vitamin K are all dependent upon functional vitamin B2.
Vitamin B12. High dose vitamin B12 has the potential to increase melatonin levels, and to also have a beneficial effect as far as modulation of the immune response. Vitamin B12 has also been demonstrated to inhibit the RNA-polymerase activity of the nsp12-protein from COVID-19 (Narayanan and Nair 2020)
Iron. Iron deficiency has been associated with an increased susceptibility to respiratory infections (Jayaweeraetal, 2019). High dose vitamin B12 has the potential to increase melatonin levels, and to also have a beneficial effect as far as modulation of the immune response.
Melatonin. There is the potential to give melatonin to increase the resistance to COVID-19. Doses of 3, 6 and 10 mg, have been given to patients in ICU, were found to be safe. Further doses of 1 g per day have been given for a month with no effect (Zhang etal 2020)..
General. Some general information on nutrition and fight COVID-19 has been summarized by Zhang and Liu (2020). Unfortunately, as long as the medical profession refuses to accept the importance of minerals such as Selenium, and vitamins D, B12 and B2 and iron in increasing the resistance to viral infections and in controlling the severity of infections, they will never recommend supplements as a preventative option against infection. Potentially simple supplementation with vitamin D, to double population levels, supplementation with Selenite, to double the population levels, and topical or injected vitamin B12 could have reduced the death rate from COVID-19 to one eighth of the current rate, potentially saving over 200,000 lives.
Long COVID
The "fight" against COVID involves sequestration and utilization of vitamins such as vitamin D, vitamin B2, vitamin B12 as well as iron. Levels of serum Ferritin are greatly increased during, and following, COVID infection. Potentially the higher need for Selenium for the Selenoprotein Glutathione Peroxidase, would lead to reduced available Selenium for enzymes such as Selenium is required for the enzyme Iodothyronine deiodinase, which in turn would lead to lower activation of vitamin B2, to FMN and then FAD. Energetically huge amounts of vitamin B2 and B12 are utilized in the "fight" against COVID, and after the infection people who recover can have greatly depleted levels of these vitamins, and those with higher susceptibility to the virus are likely more to suffer long term effects, including prolonged Chronic Fatigue like symptoms - also known as Long COVID. In this regard, symptoms are very similar to ME/CFS, and include fatigue, brain fog, myalgia, headache, dizziness, breathlessness, palpitations, anosmia and gastrointestinal problems (McCaddon and Regland, 2021). Recovery from long COVID therefore involves similar treatment to that for CFS. Functional B2 must be restored, which may involve supplementation with Iodine, Selenium and/or Molybdenum, as well as administration of high levels of vitamin B12, and vitamin D. Assessment of deficiency can be achieved by Organic Acids Test (Great Plains Laboratories), HMTA (DData), and normal blood tests, particularly TSH/T4/T3. Potentially, the normal innate immune mechanisms, one of which is the production of Xanthine Oxidase, could drain levels of Molybdenum and so exacerbate Long COVID due to lack of activation of FAD Synthase due to local Molybdenum deficiency (Skulachev, 1998).
Mechanism of invasion of COVID-19
Video of the mechanism behind severe systemic inflammatory response syndrome with COVID-19
https://www.youtube.com/watch?v=PWzbArPgo-o
Review of Statistics on outbreak in China
See https://www.worldhealth.net/news/risk-factors-covid-19-related-death-identified/
Co-morbidities raise the risk of death from Corona. Thus, in China the death rate in those with no co-morbidities was 0.9%, but was much higher for those with Cardiovascular disease (10.5%), diabetes (7.3%), Chronic respiratory diseases (such as COPD, 6.3%), Hypertension (6.0%) and cancer (5.6%). In many countries, including the US, many people in the population have at least one underlying health condition (US, 60%).
Review of Statistics on outbreak in Great Britain
The progression of the disease can lead to a critical point in which a decision must be made as to whether to admit the patient to critical care. See an explanation of the virus and who it infects and kills from a summary of UK Data
Review of Statistics on outbreak in New York
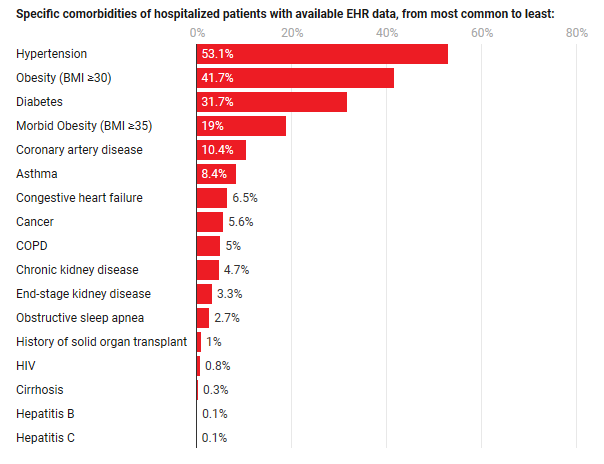
In common with the statistics from both China and UK, the greatest death rate was seen in persons with more than one risk factor. Frequency of comorbidities was Hypertension (57%), Obesity (41.7%), Diabetes (31.7%), Morbid Obesity (19%), Coronary Heart Disease (10.4%), Asthma (8.4%). Each condition, can also be shown to be associated with functional vitamin B2 deficiency, and as such could also be associated with Selenium deficiency, however, neither functional B2 levels or Selenium levels have been measured in the patients, nor those that succumbed to the infection. It can be seen, that the hospitalization rate for people
Coranavirus Vaccine
Many researchers are of the belief that there is every reason to believe that it should be possible to develop a coronavirus vaccine for humans, as many individuals who have been infected with the virus recover, and over 90% of those infected in China have now recovered. Further, it is known that passive immunity gained from bovine colostrum will protect calves against bovine coronavirus, if the titre is high enough (Bok etal, 2018). Recently Moderna has generated an mRNA vaccine against COVID-19. Best estimates for a vaccine to be on the market are still 18 months. Potential problems for the vaccine would be lack of immunogenicity in all persons. Thus, even for well established viral vaccines such as Hepatitis B, even after 3 injections there is less than a 90% seroconversion rate. Similarly, vaccine effectiveness for the common flu vaccine is only 19-60%, however, this is to a continually evolving flu virus, with effectiveness higher, the higher the similarity of the vaccine to the current flu virus. Whether COVID-19 will do that, is not known (https://www.cdc.gov/flu/vaccines-work/effectiveness-studies.htm ). Recently an analysis has been performed looking at the immunological response to hepatitis B vaccine (Yang etal, 2016), where the data looked very similar to that observed for the current COVID-19 outbreak. Thus, the vaccine was much more effective in the young, with protection more effective in females than males, and less effective in those with concomitant diseases, with a BMI >25 or those who smoked. Epitope mapping has identified potential peptide sequences that could be incorporated in a subunit vaccine, which if successful could be more rapidly scaled up than a whole viral vaccine (Feng etal, 2020). Vaccine trials have already been performed in monkeys, where it was found that severity of infection was dependent upon viral titers, so even in these preliminary trials they did not get 100% protective immunity (Barouch 2020).
Other Strategies
Several alternative strategies are possible which would potentially ameliorate the condition and reduce mortality
-
Antivirals - currently none seem to be working.
-
Peptide mimetics. Small peptides, that either mimic the binding site on ACE2, could potentially neutralize the viral binding protein, and reduce infectivity. These can be produced at large scale, however, it would not be possible to deliver these orally so that would need to be administered by injection, or via technologies such the TransdermOil™ technology.
-
Anti-scabies treatment. A group in Melbourne Australia has found that a single dose of the drug Ivermectin could stops SARS-COV2 virus in culture (Caly etal, 2020)
Treatment with Melatonin
Given the possible association of decreasing melatonin with age, and raising death rate with age, combined with the known anti-inflammatory effect of melatonin and its ability to down-regulate the innate response and the excess inflammatory response to viral infections (Reiter etal, 2017), it has been postulated that high dose melatonin may be an effective adjunct therapy in treatment of COVID-19 (Reiter etal, 2020; Zhang etal, 2020; Anderson and Reiter, 2020).
Comparison to Flu
It would seem useful to compare Coronavirus to the Flu. The annual burden of Flu in the US since 2010 has been between 9,300,000 to 45,000,000. Of these there were 140,000 to 810,000 hospitalizations with an annual death rate of 12,000 to 61,000 (CDC). Claims are that Coronavirus is different to flu in that the death rates for flu are in both the young and old. Globally, however, death rates go up for flu. <65 years - 0.1 to 6.5 per 100,000; 65-74 years 2.9-44.0 per 100,000 and for over 75, 17.9 to 223.5 per 100,000 (0.234%) (Iuliano etal, 2018). it is not known if susceptibility to COVID-19 is related to blood type, however, it has been shown in many studies that susceptibility to Influenza virus is, with type B and AB being much less able to generate effective antibody responses to Influenza A. Preliminary studies from China suggest that susceptibility to COVID-19 may be slightly higher in type A blood types. These data support the general concept that one's ability to fight the infection is affected by one's genetics (see section above on Vaccine).
Diseases of Aging
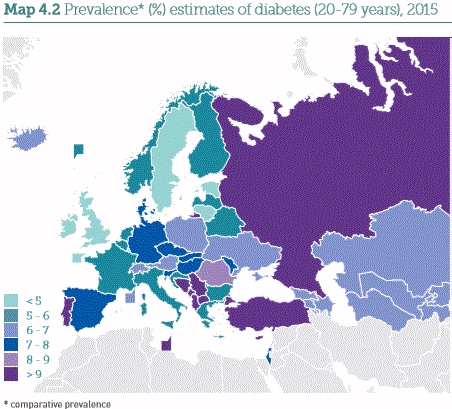
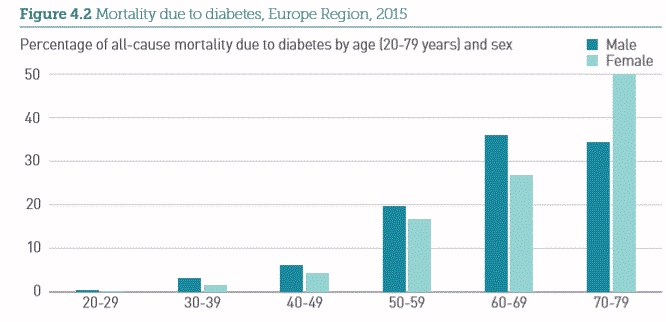
Potentially the increased mortality from Coronavirus could be simply due to the increase in the incidence of the many comorbities for death from COVID-19 with aging, and would suggest that people who have exercised often, and maintained healthy life-style and hence have no co-morbidities are being rewarded for their life-time of healthy living by having a low mortality rate from the virus. In contrast those who have not taken care of their health have an increased mortality rate, which increases rapidly with more and more comorbidities. It may not be quite to straight forwards, because if that was the case, one would expect that in Europe, the countries with the highest rates of Hypertension, Obesity, Diabetes, Morbid Obesity, and Coronary Heart Disease should have the highest death rates. This does not appear to be the case, however. Thus if you look at the incidence of Diabetes, it does increase with age, however, death from diabetes in Europe, UK and Sweden have some of the lowest death rates from diabetes, yet the highest death rate from COVID-19.
Testing
Currently the majority of tests for Coronavirus test whether you have a detectable amount of the virus. The results of the test are being widely misunderstood to mean that the person does not have the virus, whereas this may not be true. All the test means is that at the time of testing the person being tested had undetectable amounts of the virus. It does not mean that if you tested the same person 4 or 5 hours later, they would still test negative for the virus.
Research
Spike Proteins See Link
References
Covid and ACE-2 receptors: https://www1.racgp.org.au/newsgp/clinical/ace-inhibitors-arbs-and-covid-19-what-gps-need-to?feed=RACGPnewsGPArticles
Wu etal Melatonin receptor agonist protects against acute lung injury induced by ventilator through up-regulation of IL-10 production. Resp Res (2020)
Wheatley C. A Scarlet pimpernel for the resolution of inflammation? The role of supra-therapeutic doses of cobalamin, in the treatment of Systemic Inflammatory Response Syndrome (SIRS), Sepsis, severe Sepsis and Septic or Traumatic Shock. Med Hypoth 2006 67, 134-42
Seko etal, Inhibition of angiotensin-converting enzyme by selenoneine. Fisheries Science, 2019 85, 731-736
Manzanares and Hardy. Vitamin B12: the forgotten micronutrient for critical care. Curr Opin Clin Nutr Metab Care, 2010 13, 662-8
Hoffmann and Berry. The influence of selenium on immune responses. Mol Nutr Food Res 2008, 52, 1273-1280 https://www.ncbi.nlm.nih.gov/pubmed/18384097
Beck MA, Levander OA, Handy J. (2003) Selenium deficiency and viral infection. J Nutr. 133:1463S-1467S. https://www.ncbi.nlm.nih.gov/pubmed/12730444
Beck etal. Selenium deficiency increases the pathology of an influenza virus infection. FASEB J 2001 15; 1481-3
Beck etal Benign human enterovirus becomes virulent in Selenium deficient mice. J. Med Virol 1994 43; 166-70
Steinbrenner H, Al-Quraishy S, Dkhil MA et al. (2015) Dietary selenium in adjuvant therapy of viral and bacterial infections. Adv Nutr. 6:73-82.
https://www.ncbi.nlm.nih.gov/pubmed/25593145.Hurwitz etal. Suppression of human immunodeficiency virus type 1 viral load with Selenium supplementation... Arch Int Med, 2007, 167, 148-54
Baum etal. High risk of HIV-related mortality is associated with selenium deficiency. J Acquir Immune Defic Syndr Hum Retrovirol 1997 15; 370-4
Zhang etal, 2016 Decreased levels of vitamin B12 in aging, autism and schizophrenia.
PMID: 26799654Escames etal. Pharmacological utility of melatonin in the treatment of septic shock: Experimental and clinical evidence. J Pharm. Pharmacol. 2006a 58: 1153-65
Lopez etal Identification of an inducible nitric oxide synthase in diaphragm mitochondria from septic mice.... Int J Biochem Cell Biol 2006b 38, 267-78
Carrillo-Vico etal. Beneficial peleotropic actions of melatonin in an experimental model of septic shock in mice.... J Pineal Res 2005 39, 400-8
Srinivasan etal. Melatonin in septic shock: some recent concepts. J Crit Care 2010 25, 656e
Reiter etal Free redical-mediated molecular damage. Mechanisms for the protective actions of melatonin in the central nervous system. Ann NYAS 2001, 939, 200-15
Reiter etal Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas. Cell Mol Life Sci 2017 74, 3863-3881
Biancatelli etal. Melatonin for the treatment of sepsis: the scientific rational. J Thorac Dis 2020 12: S54-S65
Favero etal Melatonin as an Anti-inflammatory agent modulating inflammasome activation. Int J Endocrinol. 2017 2017:1835195
Abgstrwurm etal Selenium in Intensive care..... Crit Care Med 2007 35, 118-26
Kurniawan etal. Glutathione restricts serine metabolism to preserve regulatory T cell function. Cell metabolism. 2020, doi.org/10.1015/j.cmet.2020.03.004
Carnesecchi etal NADPH Oxidase-1 plays a crucial Role in Hyperoxia-induced acute lung injury in mice 2009. rccm.200902-0296OC
Bailey etal. The epidemiology of global micronutrient deficiencies. Ann Nutr Metab. 2015 66; 22-33
Stepan etal. Implications of the iron deficiency in lower tract respiratory acute infections in toddlers. Curr Health Sci J. 2018 44; 362-367
Tansarli etal Iron deficiency and susceptibility to infections: Evaluation of the clinical evidence. Eur J. Clin Microbiol Infect Dis. 2013, 32; 1253-8
Bai etal . Clinical characteristics of 14 critically ill children with 2009 Infuenza A (H1N1). Zhonghua Er Ke Za Zhi 2010 48; 860-4
Lakhan etal Retrospective review of factors associated with severe hospitalised community-acquired influenza... Inf Other Resp Vir 2016, 10; 476-485
Nickol etal. A cross-sectional study of the prevalence and associations of iron deficiency in a cohort of patients with chronic obstructive pulmonary disease. BMJ Open 2015 5 e007911
De Silva etal. Iron supplementation improves iron status and reduces morbidity in children with or without upper respiratory tract infections:.. Am J Clin Nutr 2003 77; 234-41.
Yu etal. A review of the novel application and potential adverse effects of proton pump inhibitors. Adv Ther 2017 34, 1070-1086
Hurrell RF Iron fortification: its efficacy and safety in relation to infections. Food Nutr Bull 2007 29, S585-94
Semba RD. Vitamin A and immunity to viral, bacterial and protozoan infections. Proc Nutr Soc 1999, 58; 385-392
Lee etal. Effects of dietary vitamin A content on antibody responses of feed-lot calves inoculated intramuscularly with an inactivated bovine coronavirus vaccine. Am J Vet Res 2013, 75;1353-1352
Hemila H. itamin C and SARS coronavirus. J Antimicrob Chemother 2003, 52:1049-50
Atherton etal. The effect of ascorbic acid on infection chick-embro ciliated trachael organ cultures by coronavirus. Arch Virol. 1978; 56, 195-199
Nonnecke etal, 2014; 97, 5566-5579.
Zhang et al. COVID-19; Melatonin as a potential adjuvant treatment Life Sci
Zhang etal. Association between regional Selenium status and reported outcome of COVID-19 cases in China. Am J Clin Nut
(thanks to J Frick)Reiter etal, 2020 https://www.frontiersin.org/articles/10.3389/fmed.2020.00226/full?fbclid=IwAR1Ol2f5qqWAJJTUS4biFzQw3xQnzdridTi22BLXtRVRmZOALeTI2zhRc2U#F2
Zhang and Liu Potential interventions for novel coronavirus in China: A systematic review. J Med Virol 2020 https://doi.org/10.1002/jmv.25707
Rayman etal. Association between regional selenium status and reported outcome of COVID-19 cases in China. Am J. Clin Nut 2020.DOI: 10.1093/ajcn/nqaa095
Carnesecchi etal Martineau etal Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 2017 346
Parinandi etal. Hyperoxia-induced NAD(P)H oxidase activation and regulation by map kinases in human lung endothelial cells. Am J. Physiol 284: 128 - L26-28
Ginde etal. Association between serum 25-hyroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 2009 169:384-390
Joliffe etal, Vitamin D in the prevention of acute respiratory infection. Systematic review of clinical studies. J Steroid Biochem Mol Biol 2013; 136, 321-329
Bjelakovic etal Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Sys Rev. 2011 PMID 21735411
Evidence that vitamin D supplementation could reduce the risk of Influenza and COVID-19 infections and death https://www.ncbi.nlm.nih.gov/pubmed/32252338
Sizar etal Vitamin D Deficiency 2020 https://www.ncbi.nlm.nih.gov/books/NBK532266/
https://www.ncbi.nlm.nih.gov/21310306
Ireland Vitamin D https://tildo.tcd.ie/publications/reports/pdf/Report_Covid19VitaminD.pdf
John Campbell Utube discussion https://www.youtube.com/watch?v=GCSXNGc7pfs&t=1s
https://www.research.square.com/article/rr-21211/v1
https://www.ncbi.nlm.nih.gov/pmc/article/PMC5954269/
Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the
severity of COVID-19? Clin Med (Lond). 2020 Jul;20(4):e107-e108. doi:
10.7861/clinmed.2020-0301. Epub 2020 Jun 5.
PMID: 32503801 Free PMC article.
De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA.Serum 25(OH)D Level
on Hospital Admission Associated With COVID-19 Stage and Mortality. Am J Clin
Pathol. 2021 Feb 11;155(3):381-388. doi: 10.1093/ajcp/aqaa252.
PMID: 33236114 Free PMC article.
Xu Y, Baylink DJ, Chen CS, Reeves ME, Xiao J, Lacy C, Lau E, Cao H. The
importance of vitamin d metabolism as a potential prophylactic, immunoregulatory
and neuroprotective treatment for COVID-19. J Transl Med. 2020 Aug 26;18(1):322.
doi: 10.1186/s12967-020-02488-5.
PMID: 32847594 Free PMC article. Review.
Skulachev, VP. Possible role of reactive oxygen species in antiviral defense. Biochemistry (Mosc). 1998 Dec: 63912):1438-40 PMIDP9916163
Pizzini A, Aichner M, Sahanic S, Böhm A, Egger A, Hoermann G, Kurz K, Widmann G,
Bellmann-Weiler R, Weiss G, Tancevski I, Sonnweber T, Löffler-Ragg J. Impact of
Vitamin D Deficiency on COVID-19-A Prospective Analysis from the CovILD
Registry. Nutrients. 2020 Sep 11;12(9):2775. doi: 10.3390/nu12092775. PMID:
32932831 Free PMC article.
Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and
severity. J Infect Public Health. 2020 Oct;13(10):1373-1380. doi:
10.1016/j.jiph.2020.06.021. Epub 2020 Jun 20. PMID: 32605780 Free PMC article.
N Basaran, M Adas, Y Gokden, N Turgut, T Yildirmak, G Guntas The relationship between vitamin D and the severity of COVID-19 Bratisl Lek Listy 2021;122(3):200-205. doi: 10.4149/BLL_2021_034. PMID: 33618529 DOI: 10.4149/BLL_2021_034
Feng etal 2020 https://www.biorxiv.org/content/10.1101/2020.03.03.962332v1.full.pdf
Bok etal, Passive immunity to control bovine coronavirus diarrhea in a dairy herd in Argentina. Reve Argent Micobiol 2018 51, 23-30.
Moderna https://time.com/5790545/first-covid-19-vaccine/
CDC https://www.cdc.gov/flu/about/burden/index.html
Iuliano etal Estimates of global seasonal Influenza - Associated respirator Mortality: A modelling study. Lancet 2018, 391; 1285-1300 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5935243/pdf/nihms962240.pdf
Barouch. Monkey vaccine trial 2020 https://www.msn.com/en-au/news/world/monkeys-resist-virus-re-infection-after-vaccine-study-immunisation/ar-BB14qGad?ocid=spartanntp
Giustina etal, 2020 https://www.bmj.com/content/368/bmj.m810/rr-36
Garami 2020 https://www.bmj.com/content/368/bmj.m810/rr-24
Phage Display
20976998-selection-sars-coronavirus-specific-cell-epitopes-phage-peptide-library-screening-evaluation-immunological-effect-epitope-based-peptides-miceCaly etal, The FDA-approved drug Ivermectin inhibits the replication of SARS-CoV-2 in vitro. https://www.sciencedirect.com/science/article/pii/S0166354220302011
Yang etal 2016 Factors influencing immunologic response to hepatitis B vaccine in adults https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914839/pdf/srep27251.pdf
Kim etal, Relationship between serum vitamin D concentrations and clinical outcome of community-acquired pneumonia.Int J Tuberc Lung Dis 2015 19: 729-34 PMID 25946368
Remmelts etal. Addition of vitamin D status to prognostic scores improves the prediction of outcome in community-acquired pneumonia. Clin Infect Dis 2012 55:1488-94 PMID 22942205
Leow etal 2011 Vitamin D, innate immunity and outcomes in community acquired pneumonia. Respirology 2011 16: 611-6 PMID 21244571
Mathias etal. Vitamin D deficiency in community-acquired pneumonia: Low levels of 1,25(OH)2 D are associated with disease severity. Respir Res. 2014 15-53
Vitamin D to be added to M&S bread https://www.bbc.com/news/uk-32941923
Vitamin D recommendations by UK health https://www.gov.uk/government/news/phe-publishes-new-advice-on-vitamin-d
McCaddon and Regland COVID-19: A methyl group assaults? Medical Hypotheses 149, 2021; 110543
Copyright © 2020 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited